Ever wondered why a sudden gasp for air can feel like an emergency alarm in your chest? Those moments are your lungs sending a distress signal, and the underlying cause often lies in a breathing disorder. Below we’ll break down the biology, the common culprits, and how doctors pinpoint what’s going wrong.
How Your Lungs Normally Work
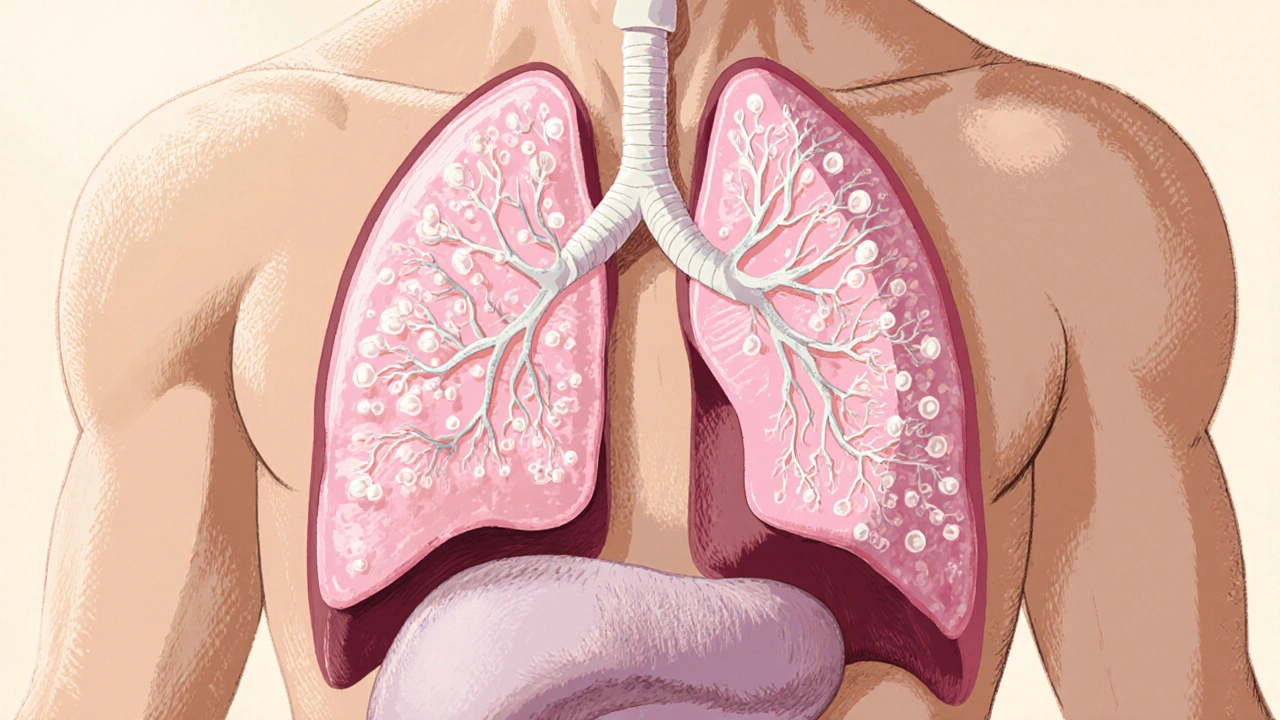
Before diving into disease, it helps to know the baseline. The respiratory system is a network of airways that brings oxygen in and pushes carbon dioxide out. Air travels down the Bronchi the two main passageways that split from the trachea into each lung, branching into smaller bronchioles that end in tiny air sacs called Alveoli cup‑shaped structures where oxygen diffuses into the bloodstream and carbon dioxide is expelled. A single healthy lung contains roughly 300 million alveoli, providing a massive surface area-about the size of a tennis court-for gas exchange.
During inhalation, the diaphragm contracts, expanding the chest cavity and lowering pressure inside the lungs. This pressure drop draws air through the airway tree. When you exhale, the diaphragm relaxes, and the elastic recoil of lung tissue pushes air out, carrying waste gases away.
Defining Breathing Disorders
Breathing disorders a group of conditions that impair the ability to move air in and out of the lungs efficiently range from mild, intermittent episodes to chronic illnesses that limit daily activities. The root problems usually involve one or more of these mechanisms:
- Airway narrowing or blockage
- Inflammation and tissue remodeling
- Loss of lung elasticity
- Impaired gas exchange at the alveolar level
- Neuromuscular control issues
When any of these fail, the body struggles to maintain adequate oxygen levels (hypoxemia) or to clear carbon dioxide (hypercapnia), leading to the characteristic breathlessness.
Common Types of Breathing Disorders
While there are dozens of specific diagnoses, four stand out because they affect millions worldwide.
Asthma
Asthma a chronic inflammatory disease of the airways that causes reversible narrowing and heightened sensitivity to triggers often begins in childhood but can persist or develop later in life. Triggers include pollen, dust mites, cold air, and exercise. During an attack, smooth muscle surrounding the bronchi contracts, mucus production spikes, and the airway wall swells, making breathing labored.
Chronic Obstructive Pulmonary Disease (COPD)
COPD an umbrella term for progressive lung diseases, primarily emphysema and chronic bronchitis, usually caused by long‑term exposure to irritants like cigarette smoke leads to permanent airway obstruction and destruction of alveolar walls. Over time, the lungs lose elasticity, making exhalation difficult and trapping air.
Pulmonary Fibrosis
Pulmonary fibrosis a condition where lung tissue becomes scarred, thickening the interstitium and stiffening the lungs reduces the ability of alveoli to expand. Even though the airways may stay open, the stiff tissue prevents efficient oxygen transfer.
Sleep Apnea
Not always thought of as a “lung” disease, Sleep apnea a disorder where the airway collapses repeatedly during sleep, causing brief pauses in breathing leads to intermittent hypoxia and fragmented sleep. The most common form, obstructive sleep apnea, is caused by soft tissue in the throat collapsing and blocking airflow.
What Happens Inside the Lungs During a Disorder?
Although each disease follows a unique pathway, they share a few key pathophysiological steps.
- Airway Constriction: In asthma, bronchi smooth muscle contracts, narrowing the lumen by up to 70%.
- Inflammatory Cascade: Cells release cytokines (IL‑4, IL‑5, TNF‑α) that attract eosinophils and neutrophils, further swelling the airway wall.
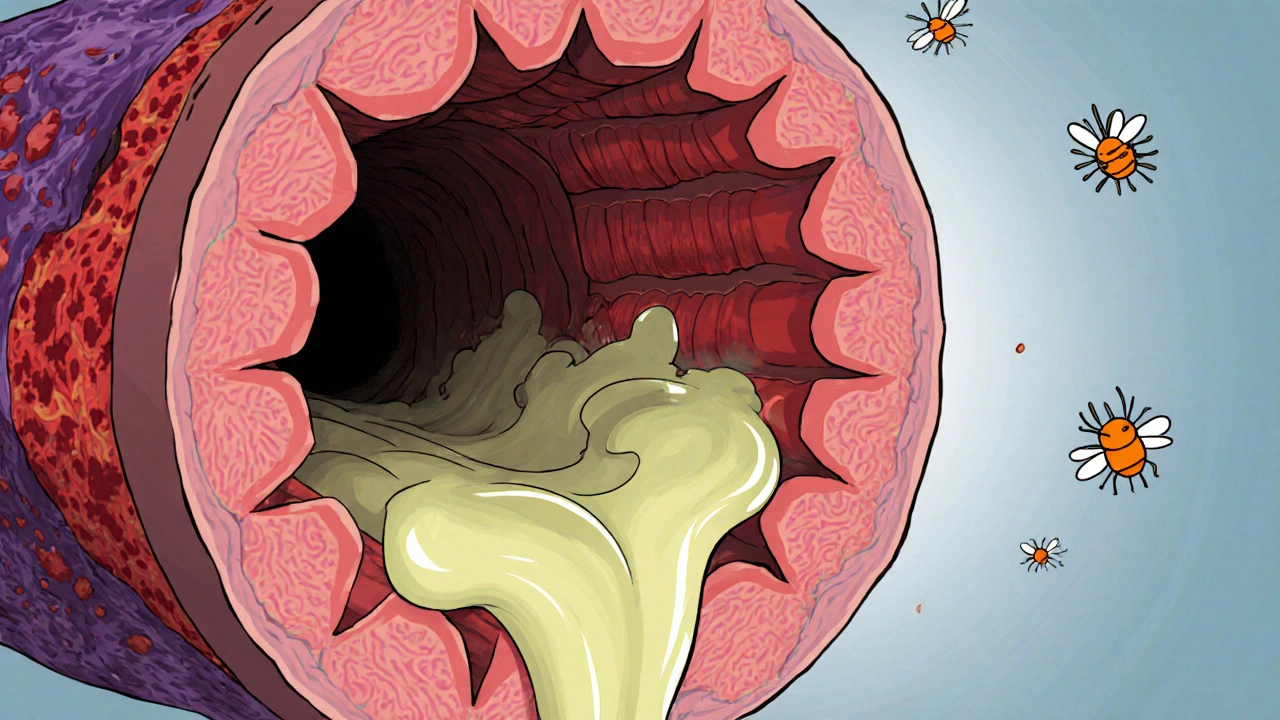
- mucus Hypersecretion: Goblet cells pump out thick mucus that clogs the bronchioles.
- Structural Remodeling: Chronic inflammation leads to thickened basement membranes and increased collagen, making the airway permanently narrower.
- Gas‑Exchange Impairment: In COPD and fibrosis, alveolar walls are destroyed or stiffened, reducing diffusion capacity (DLCO) and causing a mismatch between ventilation and perfusion.
- Ventilation‑Perfusion (V/Q) Mismatch: Some lung regions receive air but not enough blood flow, while others receive blood but insufficient air, leading to low oxygen saturation.
These changes force the respiratory muscles to work harder, which explains the tight‑chest feeling and rapid, shallow breaths patients report.
How Doctors Diagnose Breathing Disorders
Because symptoms overlap, clinicians rely on a toolbox of tests.
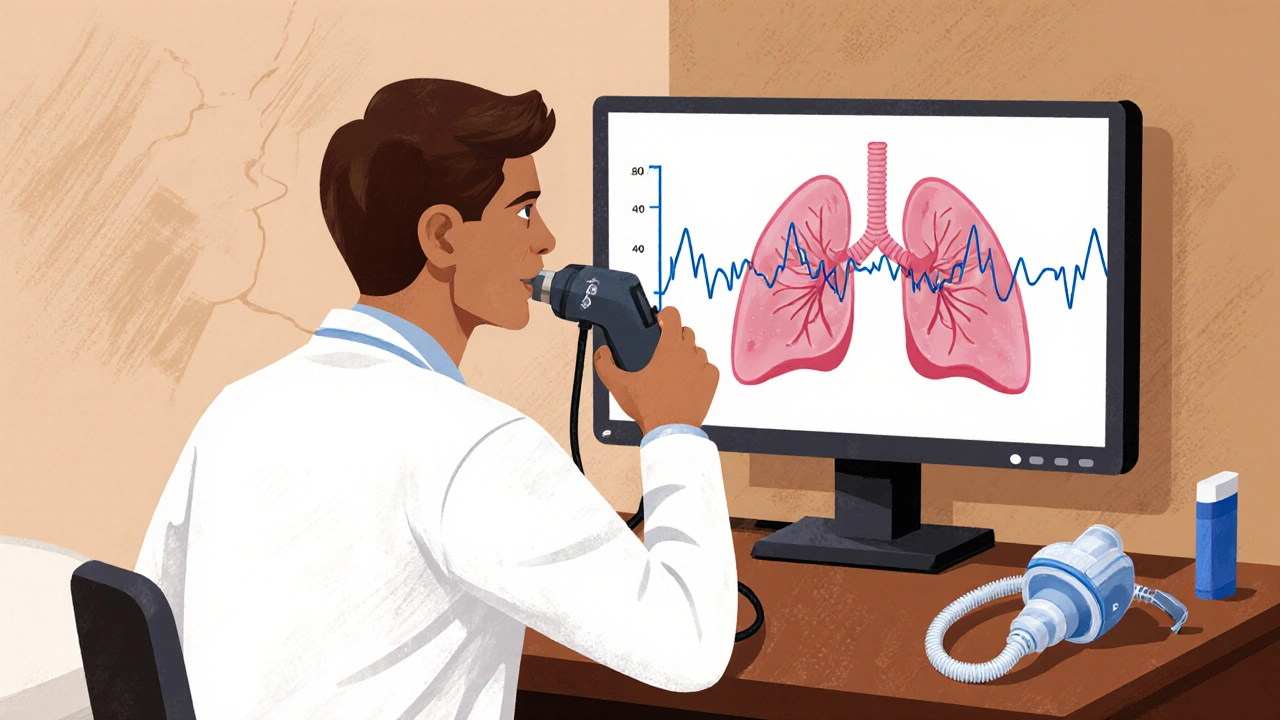
- Spirometry: Measures forced expiratory volume (FEV1) and forced vital capacity (FVC). A reduced FEV1/FVC ratio below 0.70 is a hallmark of COPD, while reversible drops after bronchodilator indicate asthma.
- Peak Flow Monitoring: Portable device that tracks maximal airflow, useful for daily asthma control.
- Chest Imaging: X‑rays reveal hyperinflated lungs in COPD; high‑resolution CT scans detect fibrotic patterns in pulmonary fibrosis.
- Oximetry and Arterial Blood Gases: Pulse oximeters give real‑time oxygen saturation (SpO2). Blood gas analysis quantifies PaO2 and PaCO2, highlighting hypoxemia or hypercapnia.
- Sleep Studies (Polysomnography): Record breathing patterns, oxygen levels, and brain waves overnight to confirm sleep apnea.
Combining history, physical exam, and these objective measures paints a clear picture of what’s happening inside the lungs.
Managing and Treating Breathing Disorders
Treatment strategies aim to restore airway patency, reduce inflammation, and improve gas exchange.
Medications
- Bronchodilators: Short‑acting (albuterol) for quick relief; long‑acting (salmeterol) for maintenance.
- Inhaled Corticosteroids: Reduce airway inflammation in asthma and sometimes in COPD.
- Antifibrotic Agents: Drugs like nintedanib slow the progression of pulmonary fibrosis.
- CPAP/BiPAP Machines: Provide continuous positive airway pressure to keep the throat open in sleep apnea.
Non‑Pharmacologic Approaches
- Smoking cessation-most effective step for COPD.
- Pulmonary rehabilitation-exercise training, breathing techniques, and education.
- Weight management-helps reduce pressure on the diaphragm, especially in sleep apnea.
- Vaccinations (influenza, pneumococcal)-prevent infections that can worsen lung function.
Advanced Interventions
- Oxygen therapy for chronic hypoxemia.
- Lung volume reduction surgery in selected emphysema patients.
- Lung transplantation for end‑stage fibrosis or severe COPD.
Choosing the right mix depends on disease severity, patient lifestyle, and comorbidities. Regular follow‑up with pulmonary function testing keeps the plan on track.
Key Takeaways
- Breathing disorders involve airway narrowing, inflammation, loss of elasticity, or impaired gas exchange.
- Asthma, COPD, pulmonary fibrosis, and sleep apnea are the most common conditions.
- Spirometry, imaging, and oxygen monitoring are core diagnostic tools.
- Treatment blends medication, lifestyle changes, and, when needed, advanced therapies.
- Early detection and consistent management can dramatically improve quality of life.
Frequently Asked Questions
Can breathing disorders be cured?
Most breathing disorders are chronic, meaning they can be managed but not fully cured. Asthma can be well‑controlled, and early‑stage COPD may stabilize with lifestyle changes, but underlying damage often remains.
Why does exercise feel harder when I have a breathing disorder?
Exercise increases oxygen demand, exposing any limitation in airflow or gas exchange. As muscles work harder, the lungs must move more air, highlighting any obstruction or stiffness.
Is it safe to use over‑the‑counter inhalers for asthma?
Only inhalers prescribed by a clinician are safe. Over‑the‑counter products lack the precise dosage and may not contain proper bronchodilators, risking inadequate relief.
How often should I get my lung function tested?
People with diagnosed breathing disorders should have spirometry at least once a year, or more frequently if symptoms change or new treatments are started.
Can diet affect my breathing?
A balanced diet supports overall lung health. Antioxidant‑rich foods (berries, leafy greens) may reduce inflammation, while excess weight can strain the diaphragm and worsen sleep apnea.








Lyle Mills
18 Oct 2025 at 17:34Inhalation dynamics hinge on diaphragmatic pressure gradients that create negative intrathoracic pressure allowing airflow into the bronchi. The bronchi branch into bronchioles which terminate in alveolar sacs lined with type I and type II pneumocytes. Gas exchange occurs across the alveolar-capillary membrane via diffusion driven by partial pressure differentials of O2 and CO2. In healthy lungs the ventilation-perfusion ratio approximates unity optimizing arterial oxygenation. When a pathology perturbs airway caliber the ratio deviates, manifesting as hypoxemia or hypercapnia. Asthmatic bronchoconstriction can reduce airway radius by up to seventy percent, dramatically increasing airflow resistance according to Poiseuille’s law. Chronic obstructive pulmonary disease induces elastic recoil loss, leading to air trapping and increased functional residual capacity. Pulmonary fibrosis replaces compliant parenchyma with collagenous scar tissue, stiffening the lungs and limiting tidal volume expansion. Sleep apnea intermittently occludes the upper airway, causing cyclic desaturations and sympathetic surges. Spirometric indices such as FEV1 and FVC quantify obstructive versus restrictive patterns. The FEV1/FVC ratio below .70 flags an obstructive defect while a preserved ratio with reduced volumes points to restriction. Arterial blood gas analysis provides PaO2 and PaCO2 values that reflect alveolar gas exchange efficiency. Imaging modalities ranging from plain radiography to high‑resolution CT delineate structural abnormalities including emphysematous bullae and fibrotic honeycombing. Therapeutic interventions target the underlying mechanism: bronchodilators relax smooth muscle, corticosteroids dampen inflammatory cascades, antifibrotics inhibit myofibroblast activity, and CPAP maintains airway patency during sleep. Lifestyle modifications such as smoking cessation and weight optimization further mitigate disease progression. Ongoing monitoring with pulmonary function tests ensures that treatment adjustments are evidence based and patient centered.