When a senior falls, the fear isn’t just about a bruise or a sprain. It’s about bleeding inside the skull, a hospital stay, or worse. For many families, that fear makes them question: Should my elderly parent be on blood thinners at all? The answer isn’t simple, but the science is clear: avoiding anticoagulants because of fall risk often does more harm than good.
Why Seniors Need Anticoagulants
About 9% of people over 65 have atrial fibrillation - an irregular heartbeat that lets blood pool and clot. Those clots can travel to the brain and cause a stroke. The risk isn’t small. At age 80 to 89, the chance of having a stroke from atrial fibrillation jumps to nearly 24% per year. That’s more than one in four people. Warfarin, used since the 1950s, cuts stroke risk by about two-thirds. Newer drugs - dabigatran, rivaroxaban, apixaban, and edoxaban - do just as well or better. They don’t need constant blood tests like warfarin. Apixaban, for example, reduced stroke risk by 21% compared to warfarin in people over 75. And it caused 31% fewer major bleeds. The BAFTA trial, which studied seniors with an average age of 81.5, found that those on anticoagulants had a 52% lower risk of stroke or systemic embolism than those on aspirin. Aspirin? It only lowers stroke risk by about 22%. For seniors with atrial fibrillation, anticoagulants aren’t optional - they’re life-saving.The Fall Risk Myth
The biggest reason doctors and families hesitate? Falls. It’s understandable. A fall on blood thinners can lead to serious bleeding. In Minnesota hospitals, 90% of fall-related deaths involved people over 85 or those on anticoagulants. That statistic terrifies everyone. But here’s what most people miss: the risk of stroke is far higher than the risk of a fatal fall. A 2023 review of 24,000 elderly patients showed that even those who’d fallen multiple times still had a net benefit from anticoagulation. The American College of Cardiology, American Heart Association, and Heart Rhythm Society all agree: fall history alone is not a reason to stop anticoagulants. In fact, the Journal of Hospital Medicine labeled stopping anticoagulants because of falls as “Things We Do for No Reason™.” Why? Because the data doesn’t support it. A senior with atrial fibrillation is more likely to have a stroke than to die from a fall. And even if they do fall, the chance of a fatal bleed is low - especially when you take steps to prevent falls in the first place.How DOACs Are Safer Than Warfarin
Older blood thinners like warfarin require frequent blood tests to keep the INR between 2.0 and 3.0. Many seniors can’t manage that. The average person on warfarin spends only 60-65% of their time in the safe range. That means they’re either underprotected or at risk of bleeding. Direct oral anticoagulants (DOACs) changed the game. They don’t need regular blood checks. Dabigatran reduces stroke risk by 88% compared to placebo. Rivaroxaban cuts intracranial bleeding by 34% compared to warfarin. Apixaban is the safest of the bunch for seniors - 31% fewer major bleeds than warfarin in those over 75. The catch? DOACs are cleared by the kidneys. As people age, kidney function drops. That’s why doctors check creatinine clearance every 6 to 12 months. If kidney function falls below 50 mL/min, doses are adjusted. For example, apixaban can be cut from 5mg twice daily to 2.5mg twice daily if the patient is over 80, weighs under 60kg, and has reduced kidney function. And if bleeding happens? Reversal agents exist. Idarucizumab reverses dabigatran. Andexanet alfa reverses rivaroxaban, apixaban, and edoxaban. These drugs became available after 2015 and are now in most hospitals. They’re not perfect, but they give doctors tools to act fast.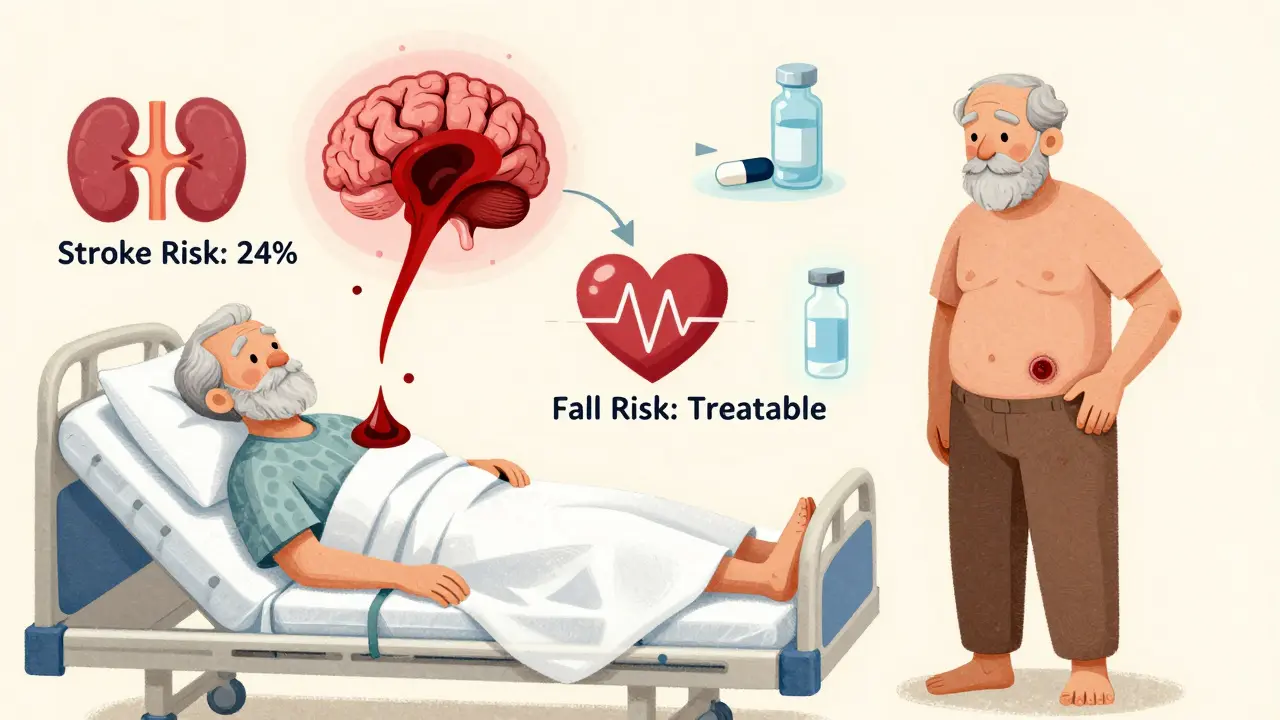
What About the Bleeding Risk?
Yes, anticoagulants increase bleeding risk. But not as much as people think - especially when you compare it to stroke risk. A 2023 analysis of octogenarians on anticoagulants found that for every 100 people treated for one year:- 24 strokes were prevented
- 3 major bleeds occurred
How to Reduce Fall Risk - Without Stopping the Meds
You don’t have to choose between stroke prevention and safety. You can have both. Start with a fall risk assessment. Tools like the Morse Fall Scale or the Hendrich II model help identify risks: poor balance, vision problems, medications that cause dizziness, or weak muscles. Then, fix what you can:- Remove tripping hazards - loose rugs, cluttered floors, extension cords
- Install grab bars in bathrooms and non-slip mats in showers
- Use bed alarms if the person gets up at night
- Review all medications. Benzodiazepines, sleep aids, and painkillers can make falls worse
- Start the Otago Exercise Program - proven to reduce falls by 35% in seniors

Why So Many Seniors Are Still Undertreated
Despite the evidence, only about 48% of seniors over 85 with atrial fibrillation get anticoagulants. That’s down from 72% in people aged 65 to 74. Why? Doctors are scared. A 2021 survey found 68% of primary care physicians would refuse anticoagulants for an 85-year-old who’d fallen twice - even if their stroke risk score (CHA2DS2-VASc) was 4, which means high risk. Families are scared too. Reddit threads are full of caregivers who were told, “Your mom falls too much - we can’t give her blood thinners.” That advice is outdated, dangerous, and not based on guidelines. The problem isn’t the drugs. It’s the fear. And the fear is fueled by misinformation.What to Do Next
If you or a loved one has atrial fibrillation and is over 65:- Ask for a CHA2DS2-VASc score. If it’s 2 or higher, anticoagulation is recommended.
- Ask if a DOAC like apixaban or rivaroxaban is right. They’re safer than warfarin for seniors.
- Ask for a fall risk assessment. Don’t accept “no” because of falls - ask what can be done to prevent them.
- Get kidney function checked every 6 to 12 months.
- Don’t stop the medication without talking to a cardiologist or geriatric specialist.
What’s Changing Now
New research is making anticoagulants even safer for seniors. The ELDERLY-AF trial is studying apixaban in people over 85. The 2024 ACC guidelines now recommend renal-adjusted dosing for DOACs in the very elderly. And AI tools are being tested to predict fall risk by analyzing walking patterns from smartwatches. The American College of Chest Physicians says it plainly: “The net clinical benefit of anticoagulation remains positive even in patients with multiple falls.” That’s not a guess. That’s data. That’s science. That’s the standard of care. Stop letting fear make the decision. Let the numbers speak.Should seniors stop anticoagulants if they fall often?
No. Falling often does not mean anticoagulants should be stopped. Studies show that the risk of stroke in seniors with atrial fibrillation is much higher than the risk of a fatal bleed from a fall. Guidelines from the American Heart Association and others state that fall history alone is not a reason to avoid anticoagulation. Instead, focus on preventing falls through home safety, exercise, and medication review.
Are DOACs safer than warfarin for elderly patients?
Yes. DOACs like apixaban, rivaroxaban, and dabigatran are generally safer than warfarin for seniors. They don’t require frequent blood tests, have fewer drug interactions, and cause fewer brain bleeds. Apixaban, in particular, reduces major bleeding by 31% compared to warfarin in patients over 75. They’re now the first-line choice for most elderly patients with atrial fibrillation.
Can anticoagulants be reversed if a senior has a bleed?
Yes. Reversal agents exist for all major DOACs. Idarucizumab reverses dabigatran. Andexanet alfa reverses rivaroxaban, apixaban, and edoxaban. These drugs are available in most hospitals and can stop bleeding within minutes. Warfarin can be reversed with vitamin K and fresh frozen plasma, but it takes longer. Reversal agents make DOACs safer than ever for seniors.
How often should kidney function be checked in seniors on DOACs?
Kidney function should be checked every 6 to 12 months in seniors on DOACs. Since these drugs are cleared by the kidneys, declining function can raise drug levels and increase bleeding risk. If creatinine clearance falls below 50 mL/min, the dose may need to be lowered. For example, apixaban can be reduced from 5mg to 2.5mg twice daily in patients over 80 with low weight and reduced kidney function.
What’s the best way to prevent falls in seniors on blood thinners?
Use a multifactorial approach: remove tripping hazards at home, install grab bars and non-slip mats, review medications that cause dizziness (like benzodiazepines), and start the Otago Exercise Program - proven to reduce falls by 35%. Bed alarms and vision checks also help. These steps are more effective than stopping anticoagulants and allow seniors to stay safe without losing stroke protection.








Pooja Kumari
10 Jan 2026 at 05:09Look, I get it - my mom fell last winter and cracked her hip, and we all panicked. But honestly? The real terror isn’t the fall. It’s waking up six months later in a nursing home because her brain got hijacked by a stroke that could’ve been stopped. I watched my aunt die from a clot while we were too scared to give her apixaban because she ‘fell too much.’ Turns out, she fell five times in two years. Five. And she had zero bleeds. But one stroke? That took her speech, her independence, her whole damn self. DOACs aren’t magic, but neither is fear. We’re treating a symptom, not the disease. And the disease is silent, slow, and lethal. Stop letting fear make medical decisions. Talk to a geriatric cardiologist, not a well-meaning cousin who watched too many medical dramas.
Also, the Otago program? My mom’s been doing it for eight months. She walks like a rockstar now. No more cane. No more wobbling. And she’s still on apixaban. No accidents. No ER visits. Just better balance, better life. Stop the meds? No. Fix the environment. That’s the real win.
And yes, kidney checks matter. We do them every six months. Simple. Free. Doesn’t take five minutes. Why are we making this harder than it is?
Stop letting fear be the doctor.
And if you think aspirin is enough? Sweetie, that’s like using duct tape to fix a cracked engine block.