Every year, millions of people in the U.S. rely on generic drugs to manage chronic conditions like high blood pressure, diabetes, and depression. These medications are cheaper, often costing 80-90% less than brand-name versions. But behind that low price tag is a complex global supply chain where contamination risks are rising - and not everyone knows how to spot them or what to do when they happen.
What Exactly Is Generic Drug Contamination?
Contamination means something unintended ends up in your pill, capsule, or cream. It could be a chemical residue from another drug made on the same machine, a tiny bit of mold, metal particles from worn equipment, or even bacteria. The FDA defines it as the undesired introduction of impurities into a drug product from the environment, other products, or the manufacturing process itself. This isn’t rare. In 2022, 22% of all drug recalls in the U.S. were due to contamination - and nearly 4 out of 10 of those recalls hit generic drugs specifically. The problem isn’t that generics are inherently unsafe. It’s that many manufacturers operate on razor-thin margins, cutting corners on cleaning, staffing, or facility upgrades to stay profitable.Where Does Contamination Come From?
Most contamination doesn’t happen by accident - it’s the result of system failures. Here are the top sources:- Cross-contamination: When one drug’s residue sticks to equipment and gets mixed into the next batch. This is especially dangerous with potent drugs like cancer treatments or hormones. The FDA requires cleaning to remove at least 10 parts per million (ppm) of previous residue, but that limit may not be enough for highly active substances.
- Microbial growth: Mold, bacteria, or yeast can grow in poorly controlled environments. For non-sterile oral drugs, the limit is 1,000 colony-forming units (CFU) per gram. Exceed that, and you risk infections or allergic reactions.
- Human error: People shed about 40,000 skin cells per minute. In cleanrooms, staff are the #1 source of particles. A single person moving around can release over 100,000 particles larger than 0.3 microns. If gowning procedures aren’t strict, those particles carry microbes into the product.
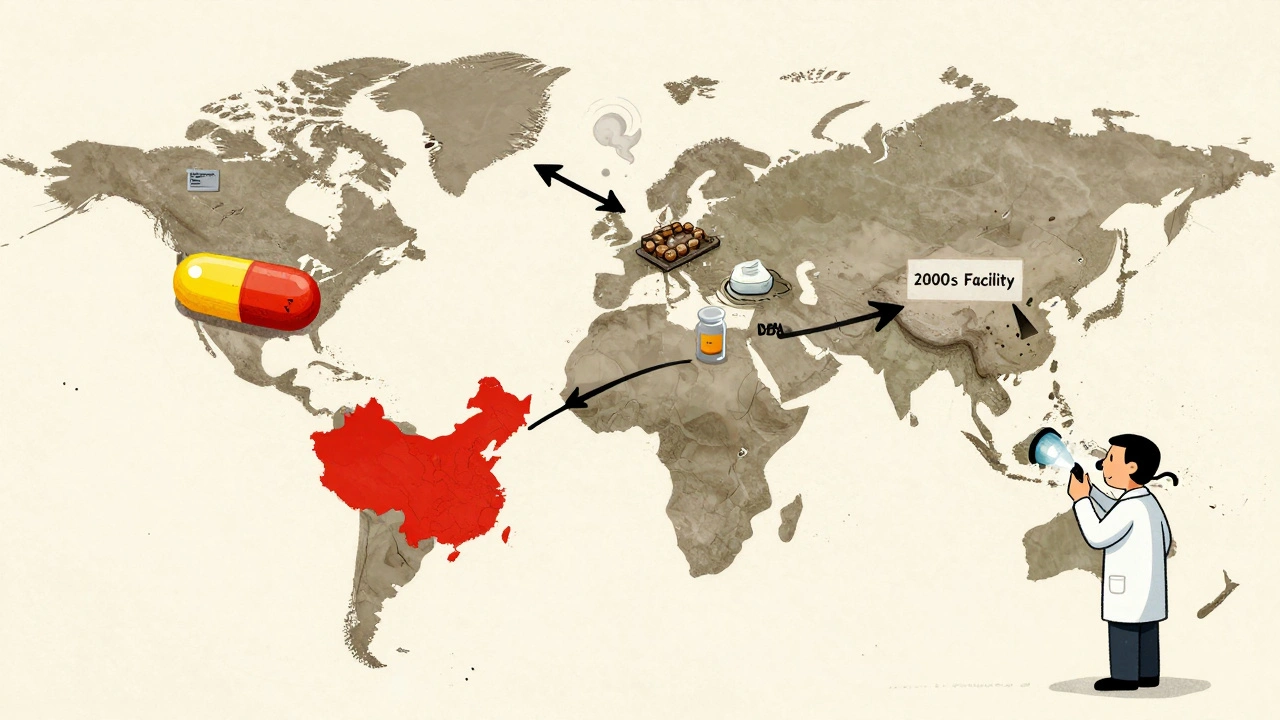
- Global supply chains: About 80% of the active ingredients in U.S. generic drugs come from just two countries - India and China. The FDA inspects only 1% of imported drug facilities each year. That means most contamination goes undetected until it hits pharmacy shelves.
- Outdated facilities: Plants built before 2000 are 34% more likely to have contamination issues. Older ventilation, poor airflow, and worn surfaces make it harder to keep environments clean.
Why Are Generic Drugs More at Risk?
Generic manufacturers face pressure that brand-name companies don’t. While brand-name drugs have profit margins of 60-70%, generics average just 20-25%. That means:- Less money for advanced cleaning systems
- Fewer staff trained in contamination control
- Delayed upgrades to ISO Class 5 cleanrooms for sterile products
- Slower adoption of rapid testing tech that cuts detection time from 7 days to just 4 hours
Real Cases: What Contamination Looks Like
The FDA’s MedWatch database recorded over 1,200 reports of suspected contamination between 2020 and 2022. Here are a few real examples:- A patient developed severe skin rashes after using a generic hydrocortisone cream. Testing found copper particles - likely from corroded pipes in the manufacturing plant.
- A pharmacist in Ohio noticed blue specks in metronidazole tablets. Lab tests confirmed copper contamination, possibly from faulty mixing equipment.
- In 2018, a global recall of blood pressure meds (valsartan) exposed nitrosamine impurities linked to carcinogens. Twenty-two generic makers were affected across eight countries. The cost? Over $1.2 billion in recalls and lost sales.
How Manufacturers Prevent Contamination
The good news? Many companies are fixing these problems. Here’s how the best ones do it:- Closed manufacturing systems: Instead of open mixers and transfer lines, top manufacturers use sealed, automated systems that keep products isolated from air and people. Teva’s facility in Italy cut cross-contamination by 78% using this method.
- Real-time monitoring: Mylan’s Morgantown plant installed sensors that track airborne particles 24/7. Alerts trigger immediate shutdowns if counts rise above safe levels.
- Advanced cleaning validation: Instead of guessing how long to clean, they test swabs from equipment after every batch. They must prove they remove residue with 95% confidence - not just hope it’s gone.
- Vertical integration: Companies that make their own active ingredients (APIs) have 22% fewer contamination incidents. Controlling the source reduces supply chain gaps.
- Rapid microbiological testing: Traditional tests take 7 days. New methods using DNA or ATP sensors give results in 4 hours. By 2022, 63% of leading generic makers had adopted them.
What You Can Do: Prevention and Response
You can’t control the factory - but you can control how you respond. If you’re a patient:- Watch for changes in your medication. New color, smell, texture, or taste? Don’t ignore it. Call your pharmacist.
- Check the FDA’s drug recall list monthly. You can sign up for email alerts at fda.gov/drugrecalls.
- Report side effects. Even if you’re not sure it’s contamination, file a report on MedWatch. One report might not matter - but 100 could trigger an investigation.
- Document unusual pills. Take photos, note lot numbers, and save samples if possible.
- Use the FDA’s Drug Supply Chain Security Act (DSCSA) to trace product origins. Every package should have a unique identifier.
- Push back on distributors pushing cheap generics with no batch history. Your reputation and your patients’ safety depend on it.
- Don’t rely on the minimum 10 ppm cleaning standard. For high-potency drugs, use toxicological risk assessments to set custom limits.
- Invest in rapid testing. The upfront cost is high, but a single recall can cost $18.7 million on average.
- Upgrade facilities. If your cleanroom is older than 2000, you’re playing Russian roulette with contamination.
What’s Changing in 2025?
The FDA isn’t waiting for more recalls. New rules are rolling out:- Since January 2023, all sartan-class blood pressure drugs must be tested for nitrosamines.
- The PREDICT system now flags 37% more risky imports than before.
- By 2024, AI-driven monitoring will analyze 15,000+ data points per facility to predict contamination risks with 89% accuracy.
- The USP updated its disinfectant guidelines - sporicidal agents are now required to kill stubborn fungal spores.
Frequently Asked Questions
How do I know if my generic drug is contaminated?
You won’t always know by looking. But if your pill looks different - new color, unusual spots, odd smell, or strange texture - don’t take it. Check the lot number against the FDA’s recall list. If you feel worse after switching to a new generic, report it to your doctor and file a MedWatch report. Contamination isn’t always obvious, but your body often reacts before labs can confirm it.
Are all generic drugs unsafe?
No. The vast majority of generic drugs are safe and effective. Over 90% of prescriptions in the U.S. are generics, and most work exactly as intended. The issue isn’t the category - it’s the manufacturer. Some companies invest heavily in quality control. Others cut corners. Your pharmacist can often tell you which brands are reliable based on their experience.
Can I test my medication at home?
No. Home testing kits don’t detect chemical or microbial contamination at the levels that matter. Only certified labs with HPLC, mass spectrometry, or microbiological culture methods can do this. If you suspect contamination, contact your pharmacist or local health department. They can help you send a sample for official testing.
Why don’t pharmacies test drugs before selling them?
Because they’re not required to - and they can’t afford to. Testing a single batch costs $500-$2,000. Most independent pharmacies don’t have the budget or equipment. The system assumes manufacturers meet FDA standards. When they don’t, the burden falls on patients and providers to notice and report problems.
What’s being done to fix this?
The FDA is using AI, better import screening, and stricter cleaning rules. Manufacturers are investing in closed systems and rapid testing. But progress is slow. The real fix requires more transparency - patients and providers need to know which generic makers have clean records. Some pharmacies now track manufacturer performance internally. Ask yours if they do.
Next Steps
If you’re taking a generic drug, here’s what to do now:- Check the lot number on your bottle. Visit fda.gov/drugrecalls and search for recalls matching your drug name and lot.
- Compare your pills to images online. Sites like Drugs.com show what approved versions should look like.
- Ask your pharmacist: "Which manufacturer makes this? Do you have any reports of issues?"
- Sign up for FDA recall alerts. It takes 30 seconds and could save your health.
- If you’ve had unexplained side effects after switching generics, report it on MedWatch. Your report matters.




Deborah Andrich
13 Dec 2025 at 08:25I’ve been on a generic blood pressure med for 5 years and never thought twice until my pharmacist flagged a batch change. Now I check lot numbers like it’s my job. Don’t wait for a reaction to act.