When your joints ache, swell, and feel stiff every morning - especially in your fingers, wrists, and knees - and you’ve been told you have lupus, it’s easy to feel overwhelmed. But here’s the reality: lupus arthritis is one of the most common and manageable symptoms of systemic lupus erythematosus (SLE). And for most people, the go-to treatment isn’t a powerful steroid or a costly biologic. It’s a simple, affordable pill called hydroxychloroquine, often sold under the brand name Plaquenil.
What Lupus Arthritis Really Feels Like
Lupus arthritis doesn’t look like rheumatoid arthritis. You won’t see bone erosion on X-rays. Instead, it’s a quiet, persistent inflammation that makes joints feel hot, tender, and stiff - especially after sitting still or waking up. About 90% of people with lupus experience this at some point. It usually hits the small joints symmetrically: both hands, both wrists, both knees. It’s not destructive, but it’s exhausting. Many patients describe it as a deep, dull ache that makes typing, gripping a coffee cup, or climbing stairs feel like a chore.
Unlike osteoarthritis, which comes from wear and tear, lupus arthritis is driven by your immune system attacking your own tissues. That’s why treating it isn’t just about pain relief - it’s about calming down the whole autoimmune response.
Why Hydroxychloroquine Is the First-Line Choice
Hydroxychloroquine has been around since the 1940s, originally developed as an antimalarial. But in the 1950s, doctors noticed something surprising: patients with lupus and rheumatoid arthritis felt better on it. Fast forward to today, and it’s the backbone of lupus treatment. According to the American College of Rheumatology, 85-90% of SLE patients take it. The European League Against Rheumatism (EULAR) gives it the highest recommendation grade - A - for every single lupus patient, no matter how mild or severe their disease.
Why? Because it does more than just ease joint pain. It reduces flares by over 50%, lowers the risk of organ damage, cuts hospital visits, and even helps you live longer. Studies show people on hydroxychloroquine have a 50% lower risk of dying from lupus complications.
How Hydroxychloroquine Actually Works
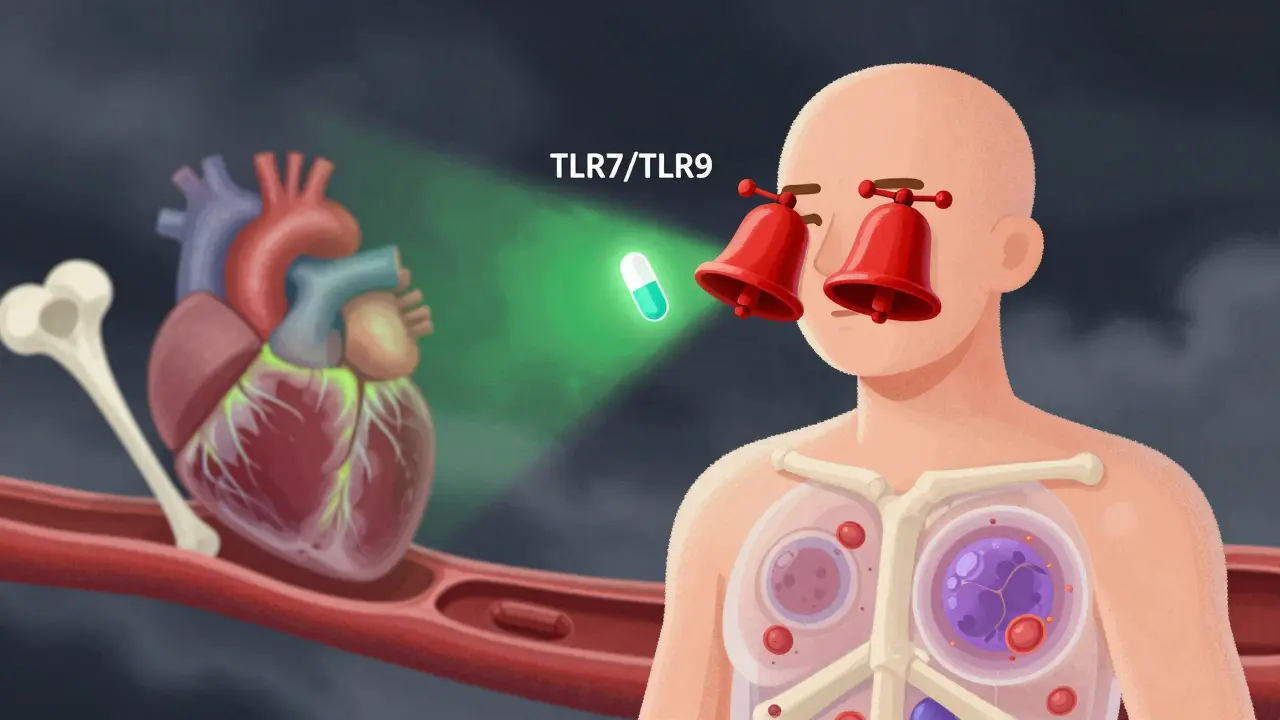
It’s not just an anti-inflammatory like ibuprofen. Hydroxychloroquine works at the cellular level. It slips into immune cells and blocks key signals that tell your body to attack itself. Specifically, it interferes with Toll-like receptors (TLR7 and TLR9), which are like alarm bells that get stuck on in lupus. By turning down these alarms, it reduces the production of interferons and TNF-alpha - two major drivers of inflammation.
It also helps clean up cellular waste by normalizing autophagy (a process that goes haywire in lupus), lowers harmful reactive oxygen species, and improves how your blood vessels function. All of this adds up to less joint swelling, fewer flares, and better long-term outcomes.
Real Benefits Beyond the Joints
What makes hydroxychloroquine unique is that it protects your whole body, not just your joints.
- Heart health: It lowers bad cholesterol (LDL) by 10-15 mg/dL and raises good cholesterol (HDL) by 5-10 mg/dL. In one 20-year study of over 2,000 lupus patients, those on hydroxychloroquine had a 44% lower risk of heart attacks and strokes.
- Blood clots: For lupus patients with antiphospholipid syndrome (a condition that increases clotting risk), hydroxychloroquine cuts the chance of dangerous clots by 30-35%.
- Bone strength: Unlike steroids, which weaken bones, hydroxychloroquine actually helps maintain bone density. One study showed a 3-5% increase in spinal bone density over two years.
- Infection risk: People taking hydroxychloroquine are less likely to get serious infections - their odds are 20 times lower than those not taking it.
This is why doctors call it the most important drug in lupus. It doesn’t just treat symptoms - it changes the course of the disease.
How It Compares to Other Treatments
Let’s say your joints are really swollen. Your doctor might consider other options:
- Methotrexate: A bit more effective for severe joint swelling, but it can hurt your liver and needs monthly blood tests. Hydroxychloroquine doesn’t.
- Biologics like belimumab: These can reduce disease activity more quickly, but they cost about $45,000 a year. Hydroxychloroquine? Around $600-$1,200 per year, even with brand-name Plaquenil.
- Corticosteroids: They work fast - in 1-2 weeks - but long-term use increases osteoporosis risk by 40%. Hydroxychloroquine takes longer, but it doesn’t cause that damage.
Hydroxychloroquine isn’t perfect for every situation. If you have severe lupus nephritis (kidney involvement), it’s not strong enough alone - you’ll need mycophenolate or other drugs. But for joint pain, fatigue, and skin rashes? It’s the gold standard.
How Long Until It Works?
This is where many patients get frustrated. Hydroxychloroquine doesn’t work like an NSAID. You won’t feel better after a few days. It takes 3 to 6 months to see real results. Some patients notice small improvements at 8-12 weeks, but full benefit often takes half a year.
That’s why adherence is so critical. About 25% of people quit within the first year because they don’t feel immediate relief. But those who stick with it? They report dramatic improvements. One patient on a lupus forum said: “After 4 months on 300mg Plaquenil, I went from needing 10mg prednisone daily to zero steroids - and my morning stiffness vanished.”
Side Effects and Safety
Hydroxychloroquine is one of the safest drugs for long-term use. The most common side effects are mild: nausea, stomach upset, or vivid dreams. These often fade after a few weeks.
The big concern? Eye damage. Long-term use can, rarely, lead to retinal toxicity. But this is extremely uncommon if you follow the rules:
- Dose is based on your real body weight: no more than 5 mg per kg per day (max 400 mg/day).
- Get a baseline eye exam within the first year.
- After 5 years of use, have an annual eye check.
- If you have kidney disease, take tamoxifen, or exceed 1,000 grams total cumulative dose, get checked sooner.
Studies show only 7.5% of people on long-term therapy develop retinal changes - and most of those are caught early thanks to screening. Only 3.2% actually have vision loss. Fear of blindness is common, but actual risk is very low when guidelines are followed.
What Patients Really Say
On CreakyJoints, 76% of lupus patients say hydroxychloroquine reduced their joint swelling. 68% say they have fewer flares. On Reddit’s r/lupus community, people regularly post: “Took 5 months to notice a difference - but now I’m 2 years in and off steroids.”
But it’s not all perfect. About 32% report side effects. Vivid dreams are the most common. Nausea happens. And yes - anxiety about eye exams is real. But most people who stick with it say the trade-off is worth it.
What You Need to Know to Use It Right
If you’re prescribed hydroxychloroquine, here’s what to do:
- Take it with food to avoid stomach upset.
- Never skip doses - consistency matters more than the exact time of day.
- Get your eyes checked as recommended - don’t wait until you have blurry vision.
- Don’t switch generic brands unless your doctor approves it. Some generics have lower blood levels, and that can affect how well it works.
- Give it at least 6 months before deciding if it’s working.
- Talk to your doctor if you’re pregnant - it’s safe and often continued during pregnancy to prevent flares.
There are tools to help. The Lupus Foundation of America offers a “Plaquenil Passport” - a printable tracker for your doses and eye exams. Over 15,000 people downloaded it in 2022.
The Future of Hydroxychloroquine in Lupus
Even after 70 years, scientists are still discovering new benefits. Recent research suggests it may influence your gut microbiome and even tweak gene expression. A 2023 study found it helps normalize interferon gene signatures - a key biomarker in lupus.
And it’s not going away. While new drugs like anifrolumab are being tested for severe cases, hydroxychloroquine remains the foundation. In Europe, 92% of new lupus patients start on it. In the U.S., it’s 85%. Even in children with lupus, it’s used in 94% of cases because it’s safer than steroids.
Its price? A few dollars a month. Its impact? Life-changing.
Final Thoughts
Lupus arthritis doesn’t have to control your life. Hydroxychloroquine isn’t a miracle cure - but it’s the closest thing we have to one for joint inflammation in lupus. It’s safe, affordable, and works on more than just your joints. It protects your heart, your bones, your blood, and your future.
If you’re on it, stick with it. If you’re not, ask your doctor why. And if you’re worried about side effects - especially your eyes - talk to your rheumatologist and get the screening you need. You’re not just treating pain. You’re protecting your whole body.




Urvi Patel
30 Dec 2025 at 14:57Look, if you're still on NSAIDs for lupus arthritis you're doing it wrong. Hydroxychloroquine isn't just a drug-it's the baseline. Anyone who says it's 'slow' hasn't lived with real inflammation. I've been on it 8 years. My joints don't scream in the morning anymore. The eye exams? Annoying but worth it. Stop treating symptoms. Start treating the disease.