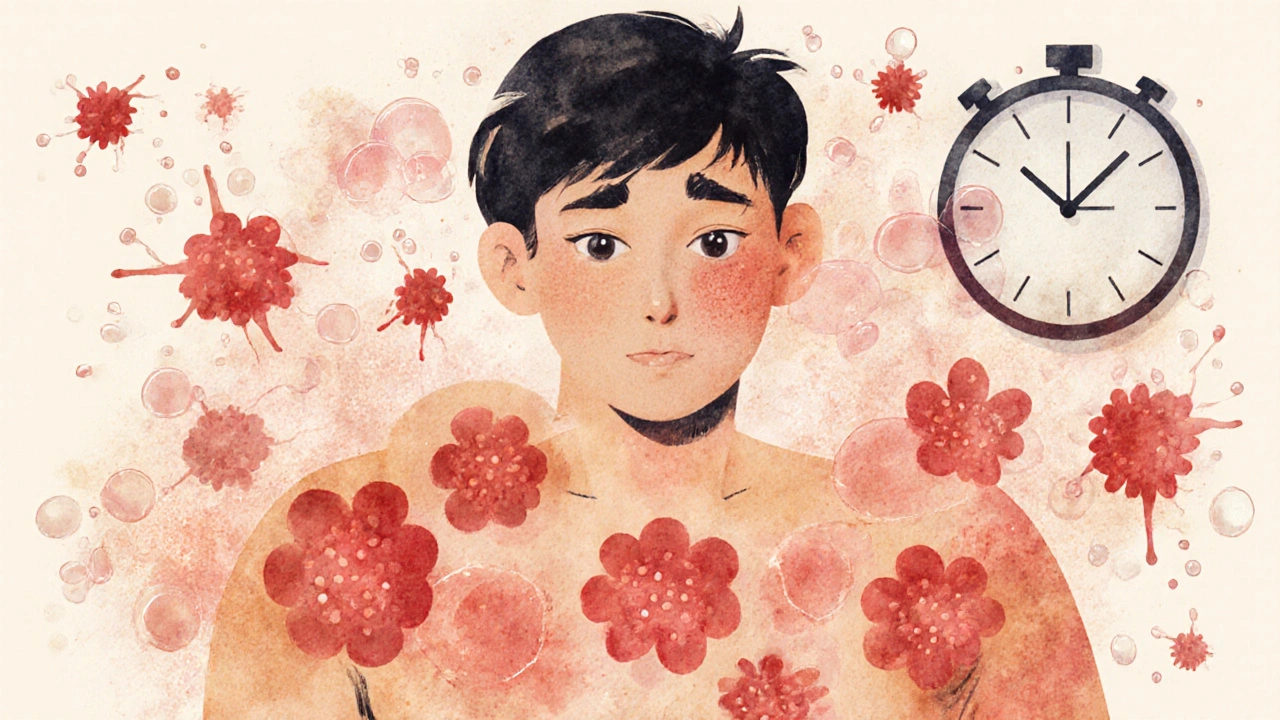
Urticaria, commonly called hives, isn’t just a rash-it’s a sudden, itchy outbreak of raised welts that can appear anywhere on your skin. One minute you’re fine, the next your arms, legs, or face are covered in angry red bumps that burn and itch. For many, these hives fade within hours. But for others, they return day after day, week after week, turning life into a constant battle with discomfort. This isn’t rare. About 1 in 5 people will deal with hives at some point in their lives, and women are more likely than men to be affected. What causes them? Why do antihistamines help? And what do you do when they don’t?
What Hives Actually Look Like and How They Form
Hives show up as raised, red or skin-colored welts that look like swollen patches. They can be as small as a pinhead or as big as a dinner plate. The edges are often sharp, and they may join together to form larger areas. What makes them so frustrating is how fast they move-they can appear in one spot, disappear in an hour, and reappear somewhere else entirely. This isn’t random. It’s your body’s immune system reacting.
Inside your skin, there are cells called mast cells. When something triggers them-like food, stress, heat, or even an unknown cause-they release histamine. Histamine makes tiny blood vessels leak fluid into the skin, causing swelling and itching. That’s the science behind the welt. The good news? It’s not contagious. The bad news? It can feel like your skin is alive and fighting back.
Acute hives last less than six weeks. Most go away on their own. Chronic hives stick around longer than six weeks, sometimes for months or even years. About 70 to 80% of chronic cases have no clear trigger. Doctors call this chronic spontaneous urticaria. It’s not allergies in the traditional sense. It’s your immune system acting up for no obvious reason.
Common Triggers: What Makes Hives Flare Up
Not all hives are the same. Some are triggered by things you can control. Others come out of nowhere.
Food allergies are a classic cause-peanuts, shellfish, eggs, and milk are common culprits. But hives can also come from medications like aspirin, ibuprofen, or antibiotics. Infections, especially viral ones like colds or flu, can trigger outbreaks too. Stress and heat are big ones. If you’ve ever broken out in hives after a hot shower or a stressful meeting, you’re not alone.
Then there are physical triggers. About 20 to 30% of chronic hives cases are tied to things like pressure (from tight clothes), cold, sunlight, or even scratching your skin. This is called physical urticaria. If you get hives after swimming in cold water or walking in the sun, your trigger might be environmental.
But here’s the catch: in most chronic cases, no trigger is ever found. That doesn’t mean it’s not real. It just means your body’s alarm system is stuck on high. And that’s where treatment becomes critical-not to find the cause, but to quiet the reaction.
Antihistamines: The First Line of Defense
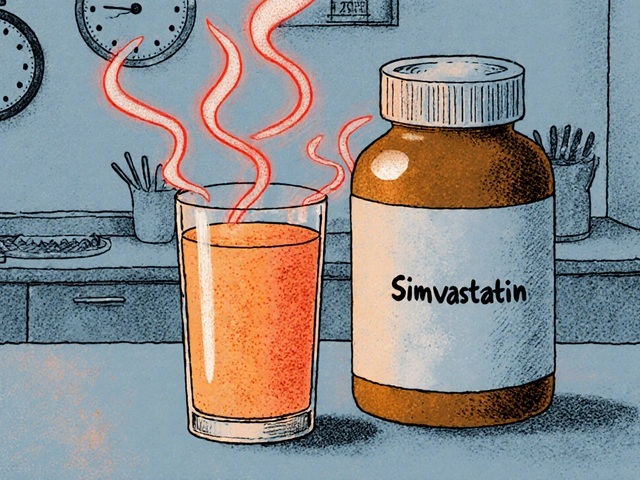
If you’ve ever taken Benadryl for hives, you’ve used a first-generation antihistamine. They work fast, but they make you sleepy-about half to two-thirds of people feel drowsy after taking them. That’s why doctors now recommend second-generation antihistamines as the go-to first step: cetirizine (Zyrtec), loratadine (Claritin), and fexofenadine (Allegra).
These don’t cross the blood-brain barrier as easily, so they don’t cause the same level of drowsiness. They’re also longer-lasting. Most people take one pill a day, and it covers them for 24 hours. Doses are usually 10mg for adults, but if that’s not enough, guidelines now say you can safely increase the dose up to four times the normal amount. That’s right-some people need 40mg of cetirizine a day to get relief.
Studies show that up-dosing helps about half of chronic hives patients who don’t respond to standard doses. And it’s safer than you’d think. Side effects are usually mild-dry mouth, headache, or tiredness. Much better than the risks of long-term steroids.
Many people swear by cetirizine for all-day control. Others find fexofenadine works better for them. It’s trial and error. If one doesn’t help after two weeks, switch to another. Don’t give up too soon.
When Antihistamines Aren’t Enough
Even with higher doses, about 40 to 50% of chronic hives patients still have symptoms. That’s where things get more serious-and more advanced.
The next step is often a biologic drug called omalizumab (Xolair). It’s an injection given under the skin every four weeks. Approved for chronic hives since 2014, it works by targeting IgE, a key player in allergic reactions. Clinical trials show it brings complete symptom control to about 65% of people who didn’t respond to antihistamines. Users on patient forums report life-changing results: no more itching at night, no more hiding under long sleeves, no more anxiety about flare-ups.
But it’s expensive-around $1,500 per shot in the U.S.-and not everyone can access it. In the UK, NHS coverage varies by region. Some patients wait months for approval.
Then came dupilumab (Dupixent), approved in September 2023. Originally for eczema and asthma, it’s now also used for chronic hives. In trials, it helped 55% of patients achieve complete relief-nearly four times better than placebo. It’s another injection, but many find it easier to tolerate than omalizumab.
And now, in January 2024, the FDA approved remibrutinib-the first oral treatment for chronic hives that targets a different part of the immune system. It’s a daily pill, not an injection. In trials, 45% of users had complete symptom control. And because it’s a pill, adherence is higher than with shots. This could change how we treat chronic hives in the next few years.
What Doesn’t Work (And Why)
Corticosteroids like prednisone can knock out hives fast. But they’re not a long-term fix. After just three days, 35% of users develop high blood sugar. 25% can’t sleep. 20% feel anxious or depressed. Doctors limit them to 3 to 5 days, max.
Cyclosporine, an immune suppressant, works for some resistant cases-but it can damage your kidneys and raise blood pressure. It’s used only when everything else fails, and patients need regular blood tests to monitor safety.
And while some people turn to natural remedies-vitamin C, quercetin, or cold compresses-there’s no solid proof they work consistently. They might help a little, but they won’t replace medicine.
Living With Chronic Hives: Real Challenges
It’s not just the itching. It’s the sleep loss. In one Reddit community with over 15,000 members, 68% said hives disrupted their sleep. Many wake up two or three times a night, scratching until their skin bleeds.
There’s also the emotional toll. Studies show 15 to 20% of chronic hives patients develop anxiety or depression. It’s easy to feel isolated when no one else can see what you’re going through. You cancel plans because you’re embarrassed. You avoid social events because you don’t know if you’ll break out.
And misdiagnosis is common. One in five people see three or more doctors before getting the right diagnosis. Hives can be mistaken for eczema, insect bites, or even a reaction to laundry detergent. That delay means months of unnecessary suffering.
Tracking your symptoms helps. Use a simple journal or a mobile app like Urticaria Tracker. Note what you ate, where you were, how stressed you felt, and when the hives appeared. Patterns emerge over time-even if you don’t find a trigger, you’ll learn what makes it worse.
What to Do Next
If you’ve had hives for less than six weeks, start with an over-the-counter antihistamine like cetirizine 10mg once daily. Take it for two weeks. If there’s no improvement, switch to fexofenadine or loratadine. Keep a symptom diary.
If hives last longer than six weeks, see a dermatologist or allergist. Don’t wait. Early intervention with up-dosed antihistamines can prevent long-term suffering. If those don’t work, ask about biologics like omalizumab or dupilumab. These aren’t last resorts-they’re proven tools.
And if you’re on steroids, ask your doctor about a plan to get off them. They’re not meant for daily use. There are better, safer options now.
The field is moving fast. New oral drugs like remibrutinib are making treatment simpler. Telemedicine is making specialist care more accessible, even in rural areas. And with more research, we’re getting closer to personalized treatment-where your genes help guide which drug works best for you.
Hives are more than a skin problem. They’re a signal. And now, we have more ways than ever to listen-and respond.
Are hives always caused by allergies?
No. While food or medication allergies can cause acute hives, most chronic cases-70 to 80%-have no identifiable allergic trigger. These are called chronic spontaneous urticaria and are linked to immune system dysfunction, not classic allergies. Physical triggers like heat, pressure, or cold can also cause hives without an allergic reaction.
Can I take antihistamines every day for years?
Yes, second-generation antihistamines like cetirizine, loratadine, and fexofenadine are safe for long-term daily use. Studies show no major risks with years of use at standard or even up-dosed levels (up to four times the regular dose). Side effects like dry mouth or mild fatigue are rare and usually mild. This is far safer than long-term steroid use.
Why do my hives get worse at night?
Hives often worsen at night due to natural changes in your body’s histamine levels and cortisol rhythms. Cortisol, which helps suppress inflammation, drops at night, making symptoms more noticeable. Also, lying down increases skin pressure and warmth, which can trigger hives in people with physical urticaria. Many doctors recommend taking a longer-acting antihistamine at night, or combining it with a short-acting one if itching keeps you awake.
Is chronic hives an autoimmune disease?
In 30 to 40% of chronic spontaneous urticaria cases, the immune system mistakenly attacks your own mast cells, making it an autoimmune condition. Blood tests can detect autoantibodies against IgE or its receptor, confirming this. But even without a positive test, the treatment approach is the same: control symptoms with antihistamines or biologics. The focus is on managing the reaction, not always finding the exact cause.
What’s the difference between hives and angioedema?
Hives affect the surface of the skin-raised, itchy welts. Angioedema is deeper swelling, often around the eyes, lips, tongue, or throat. It doesn’t always itch, but it can be dangerous if it affects breathing. Many people with chronic hives also get angioedema. If you notice swelling in your face or throat, seek medical help immediately-it could be life-threatening.
Can stress cause hives?
Yes. Stress doesn’t directly cause hives, but it can trigger or worsen them by activating the immune system. Many patients report flare-ups during periods of high stress-work deadlines, family issues, or even major life changes. Managing stress through sleep, exercise, or therapy can reduce the frequency and severity of outbreaks, even if it doesn’t eliminate them.
Are there any new treatments on the horizon?
Yes. Remibrutinib, approved in January 2024, is the first oral tyrosine kinase inhibitor for chronic hives, offering a daily pill alternative to injections. Other drugs like linzagolix are in late-stage trials and could be available by late 2024. Researchers are also exploring genetic testing to match patients with the most effective antihistamine based on their biology-personalized treatment is coming soon.
Final Thoughts
Hives can be terrifying when they first appear. But they’re rarely dangerous. And with today’s treatments, most people can find relief. The key is not to suffer in silence. Start with an antihistamine. Track your symptoms. See a specialist if they don’t improve. You don’t have to live with constant itching. Better options exist-and they’re more accessible than ever.


swatantra kumar
20 Nov 2025 at 06:54Man, I’ve been dealing with this for years and honestly? Zyrtec saved my life. Took me 3 years to figure out 20mg daily was the sweet spot. No more midnight scratching, no more hiding in long sleeves. My dog even notices when I’m clear-he’ll finally cuddle without me flinching. 🐶❤️