When you pick up a prescription at your local pharmacy, you might not think twice if the pill bottle says generic instead of the brand name. But if you’re discharged from the hospital and your heart medication suddenly changes, that’s a different story. The reason? Retail and hospital pharmacies don’t just serve different locations-they operate under completely different rules when it comes to swapping one drug for another.
How Substitution Works in Retail Pharmacies
In retail pharmacies, substitution is mostly about cost. When a doctor writes a prescription for, say, Lipitor, the pharmacist can legally switch it to atorvastatin-the generic version-unless the doctor specifically says "do not substitute" or the patient refuses. This isn’t optional; it’s standard practice. About 90.2% of eligible prescriptions in retail settings are filled with generics, saving patients and insurers billions each year. State laws give pharmacists this authority, and every state has its own rules. In 32 states, you must be told verbally that a substitution happened. In 18, you need to sign paperwork before the switch. Most patients don’t even notice-the pill looks different, but the active ingredient is the same. And for many, the lower price is a relief. A 2023 survey found that 78.3% of patients appreciate the savings. But it’s not always smooth. Insurance formularies often force substitutions. If your plan won’t cover the brand name, the pharmacist has to switch it-even if the patient is nervous. One pharmacist on Reddit shared how they spent hours calling insurers to get prior authorization for a patient who believed brand-name lisinopril worked better. That kind of back-and-forth is common. Sixty-three percent of retail pharmacists say prior authorization delays are their biggest headache.How Substitution Works in Hospitals
Hospital pharmacies don’t swap drugs at the counter. There’s no patient saying, "Can I get the cheaper version?" Instead, a team of doctors, pharmacists, and nurses decides what drugs go on the hospital’s formulary-its approved list of medications. This group, called the Pharmacy and Therapeutics (P&T) committee, meets regularly to review evidence and decide which drugs are safest and most effective for specific conditions. For example, if a patient comes in with a serious infection, the committee might approve switching from vancomycin to linezolid because studies show it’s just as effective, easier to give, and cheaper. But this decision isn’t made by the pharmacist filling the IV bag. It’s made weeks or months in advance, based on clinical data, not cost alone. And it’s not just pills. In hospitals, substitution includes IV antibiotics, biologics, and even custom-compounded drugs. About 68.4% of hospital substitutions involve non-oral medications, compared to just 2.7% in retail. That’s because hospitals treat complex cases where drug delivery matters as much as the drug itself. Every substitution in a hospital is documented in the electronic health record. If a patient’s medication changes, the system flags it for the care team. Physicians must be notified within 24 hours-required by Joint Commission standards. This isn’t about saving money; it’s about making sure every change fits into the patient’s overall treatment plan.Why the Rules Are So Different
The difference comes down to who’s making the decision-and why. In retail, the pharmacist is the last line of defense before the patient walks out the door. Their job is to ensure the right drug gets to the right person at the right price. Insurance companies drive most of the substitution decisions. If a generic is cheaper and approved, it’s usually the default. In hospitals, the pharmacist is part of a clinical team. Substitution isn’t a transaction-it’s a clinical strategy. The goal is to reduce complications, improve outcomes, and follow evidence-based pathways. A 2022 survey found that 84.6% of hospital pharmacists say patient-specific clinical factors drive their substitution choices, not insurance rules. The legal frameworks reflect this too. Retail substitution is governed by 50 different state pharmacy laws. Hospital substitution follows federal rules from CMS and standards from the Joint Commission. Hospitals also have to comply with the 340B Drug Pricing Program, which gives them discounts on drugs for low-income patients. Many hospitals use that discount to push substitutions that maximize savings without compromising care.What Happens When Patients Move Between Settings
This is where things get dangerous. A patient leaves the hospital on a new medication-maybe a different blood pressure pill than they took at home. The discharge summary says the change was made for clinical reasons. But when they get to their retail pharmacy, the pharmacist sees the original prescription and fills the old drug. Or worse, the pharmacy substitutes a different generic than what the hospital used. The Institute for Safe Medication Practices found that 23.8% of medication errors during hospital-to-home transitions involve substitution mismatches. That’s not a small number. It’s a gap in communication. That’s why more hospitals are now working with retail pharmacies. About 48.3% of hospitals have formal medication reconciliation programs that include substitution history. And 37.6% of retail chains now follow up with patients after hospital discharge to check for drug changes. These efforts are growing because they work. A 2023 APhA pilot showed that when substitution practices are aligned between settings, hospital readmissions dropped.Skills and Training: Two Different Worlds
Becoming a pharmacist in retail means learning state laws, insurance formularies, and how to explain substitutions to patients who are confused or upset. Communication skills are critical. Ninety-four percent of retail pharmacy managers say this is the most important skill for their staff. In hospitals, pharmacists need deep clinical knowledge. They have to understand drug interactions, pharmacokinetics, and how each medication fits into treatment protocols. Eighty-nine percent of hospital pharmacy directors say therapeutic expertise matters more than customer service. The learning curve reflects this. New retail pharmacists usually get comfortable with substitution in 3 to 6 months. Hospital pharmacists need 6 to 12 months to master P&T committee processes, EHR alerts, and clinical pathways.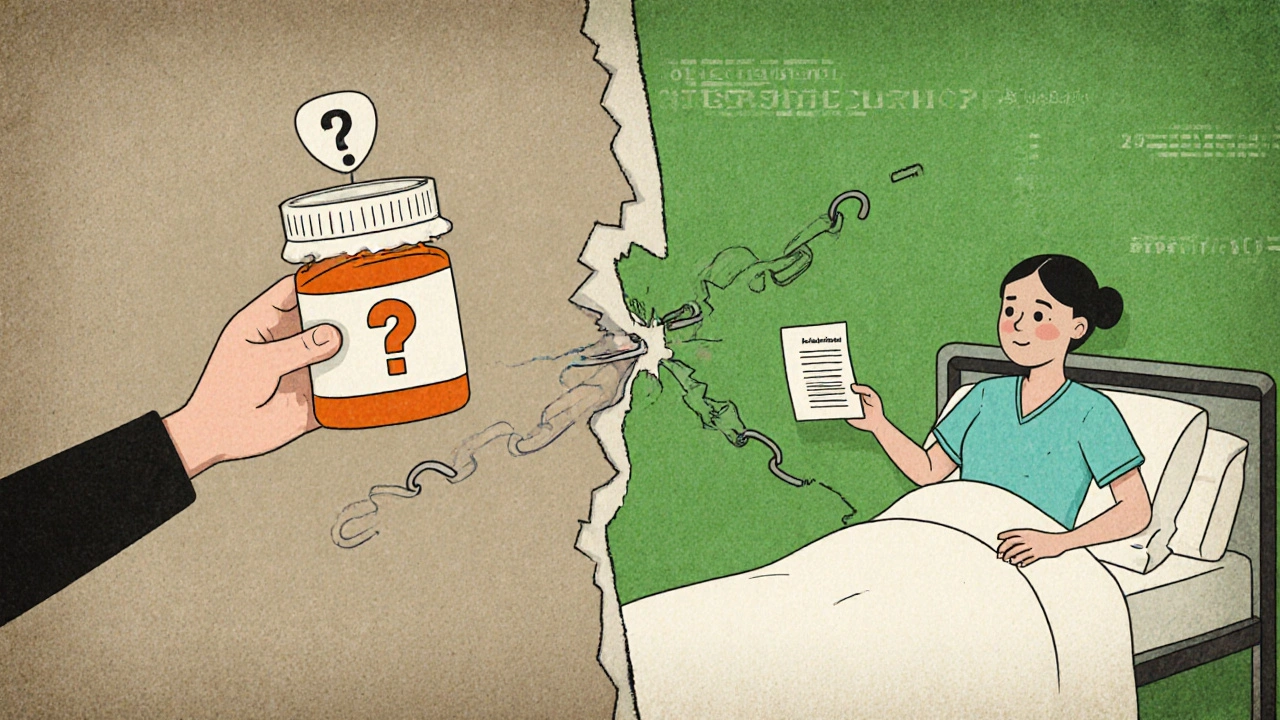
The Future: Convergence Is Coming
The two systems are starting to talk to each other. The 2023 CMS Interoperability Rule, effective July 2024, will require hospitals and pharmacies to share substitution records in a standardized format. Epic and Cerner are already building EHR modules that will let retail pharmacists see what substitutions happened in the hospital. Why? Because value-based care is changing everything. If a patient gets readmitted because of a medication mix-up, the hospital pays. So now, both sides have a financial reason to coordinate. By 2028, Avalere Health predicts 78% of healthcare systems will use integrated substitution protocols. But retail pharmacies won’t disappear as the main source of cost savings. The Generic Pharmaceutical Association estimates generic drugs will save the U.S. system $1.7 trillion by 2028-almost all of it through retail substitution.What This Means for Patients
If you’re getting a prescription filled at a store, expect a generic unless you say otherwise. Ask questions if you’re unsure. Don’t assume the new pill is the same just because it’s cheaper. If you’re in the hospital, understand that any change to your meds is likely part of a broader plan. Ask your pharmacist or nurse: "Why was this changed?" and "Will this be the same when I go home?" The system isn’t perfect. But knowing how substitution works in each setting helps you stay in control of your own care.Can a retail pharmacist refuse to substitute a generic drug?
Yes, but only under specific conditions. A retail pharmacist can refuse substitution if the prescriber writes "do not substitute" on the prescription, the patient refuses the generic, or state law prohibits it. In most cases, however, pharmacists are required to substitute unless one of these exceptions applies. Insurance formularies often make substitution mandatory, so refusal is rare.
Are hospital substitutions always cheaper than retail substitutions?
No. Hospital substitutions are primarily driven by clinical effectiveness, not cost. While many substitutions do save money, the goal is to improve patient outcomes-like reducing side effects or making treatment easier to follow. Sometimes, a hospital will switch to a more expensive drug if it’s safer or more effective. Retail substitutions, on the other hand, are almost always about lowering cost.
Why do hospitals substitute IV drugs but retail pharmacies rarely do?
Hospitals treat patients with complex, acute conditions that often require IV medications. Substituting one IV antibiotic for another can reduce complications, improve dosing accuracy, or lower infection risk. Retail pharmacies mostly fill oral medications-pills and liquids-for chronic conditions. IV drugs aren’t dispensed to patients to take home, so retail pharmacists rarely handle them. Only about 2.7% of retail substitutions involve non-oral forms.
What’s the biggest safety risk in medication substitution?
The biggest risk is when substitution practices don’t align between hospital and retail settings. A patient might leave the hospital on a new drug, but their retail pharmacy fills the old one-or a different generic. This mismatch causes about 17.4% of medication discrepancies during care transitions, according to the Institute for Safe Medication Practices. Poor communication between systems is the root cause.
Do biosimilars follow the same substitution rules as generics?
No. Biosimilars are not the same as generics. They’re complex biologic drugs that mimic other biologics but aren’t exact copies. Only 23 states have laws allowing pharmacists to substitute biosimilars without prescriber approval-and those laws vary. In hospitals, substitution of biosimilars is controlled by P&T committees. In retail, it’s often blocked by insurance policies or lack of state laws. Many patients still don’t realize biosimilars exist or how they differ from generics.









Nicole Ziegler
19 Nov 2025 at 13:34Wow this is wild 😮 I had no idea hospitals and retail pharmacies played by such different rules. Just got discharged last week and my blood pressure med switched-thought it was just the generic, but now I’m wondering if it was a clinical call. 🤔