Every time you pick up a prescription, there’s a label on the bottle. It looks simple - name, dosage, date. But hidden in that small print are critical warnings that could save your life. Every year, drug interactions send over 100,000 people in the U.S. to the hospital. Many of these cases happen because people don’t know how to read what’s on their prescription label. You don’t need a medical degree to understand it. You just need to know where to look and what to look for.
Why Prescription Labels Matter More Than You Think
Prescription labels aren’t just instructions. They’re safety tools. The FDA requires every label to include specific information about drug interactions - not as a suggestion, but as a legal requirement. That means the warnings you see are based on real clinical data, tested and approved by experts. The most dangerous interactions aren’t always obvious. For example, mixing blood thinners like warfarin with common herbal supplements like ginkgo biloba can cause internal bleeding. Yet, many patients don’t even realize supplements count as medications when it comes to interactions.Studies show that 68% of people taking five or more medications can’t identify potential interactions just by reading their labels. That’s not because they’re careless - it’s because the language is confusing. Terms like “concomitant use” or “clinically significant” aren’t everyday words. But you don’t need to memorize them. You just need to know where to find the key information.
Where to Find Drug Interaction Warnings on Your Label
Every prescription label follows a standard format set by the FDA. You’ll find interaction warnings in two main places:- Section 5: Warnings and Precautions - This is where the most serious risks are listed. If a drug can cause life-threatening reactions when mixed with another, it’s here. Look for phrases like “Avoid concomitant use with…” or “May increase risk of bleeding.”
- Section 7: Drug Interactions - This section lists all known interactions, from major to minor. It’s longer and more detailed. Pay attention to instructions like “Reduce dosage when used with…” or “Monitor for dizziness or confusion.”
Don’t skip the “Warnings” section on over-the-counter meds either. A 2023 study found that 98% of OTC products include interaction info, but only 57% of people read it. That’s a big gap. If you’re taking aspirin, ibuprofen, or even cold medicine, check the label. Mixing these with blood thinners or antidepressants can be dangerous.
What to Look for in the Wording
The FDA’s 2024 update made labels clearer. Now, manufacturers must answer three simple questions in every interaction warning:- Is there a problem? - The label will say “Avoid,” “Do not use,” or “Contraindicated.”
- How bad is it? - Look for words like “severe,” “life-threatening,” or “requires monitoring.”
- What should you do? - It should tell you: “Stop taking,” “Reduce dose,” or “See your doctor.”
For example, if your label says: “Avoid concomitant use of simvastatin with clarithromycin - risk of severe muscle damage,” that’s a clear red flag. Simvastatin is a cholesterol drug. Clarithromycin is an antibiotic. Together, they can wreck your muscles. The fix? Ask your doctor for a different antibiotic.
Another common warning: “May increase risk of bleeding when used with NSAIDs.” That means don’t take ibuprofen or naproxen with your blood thinner unless your doctor says it’s safe.
Supplements and Herbal Products Are Part of the Equation
Most people think “medication” means pills from the pharmacy. But supplements count too. Ginkgo biloba, garlic, St. John’s wort, vitamin E - these aren’t harmless. They interact with prescription drugs. A Harvard study found that 147 cases of serious bleeding were linked to warfarin users taking ginkgo biloba without telling their doctor.Here’s the problem: prescription labels only mention supplement interactions in 17% of cases. That means you have to be the one to speak up. When you see your doctor or pharmacist, say: “I take turmeric, fish oil, and melatonin.” Don’t assume they’ll ask. Most don’t.
Keep a written list of everything you take - including doses and how often. Bring it to every appointment. That simple step cuts interaction risks by 47%, according to the BeMedWise Foundation.

How to Use Tools Without Replacing Your Label
Apps like Drugs.com or Medscape can help. They’re fast and easy. But they’re not perfect. They cover 92% of prescription drugs - not 100%. And they don’t know your full medical history. Your label? It’s tailored to you. It’s the only source that’s legally required to match your exact prescription.Use apps as a second check - not your first. Enter all your meds into Drugs.com’s checker. If it flags something your label doesn’t, bring it to your pharmacist. But never ignore your label because an app says it’s “fine.”
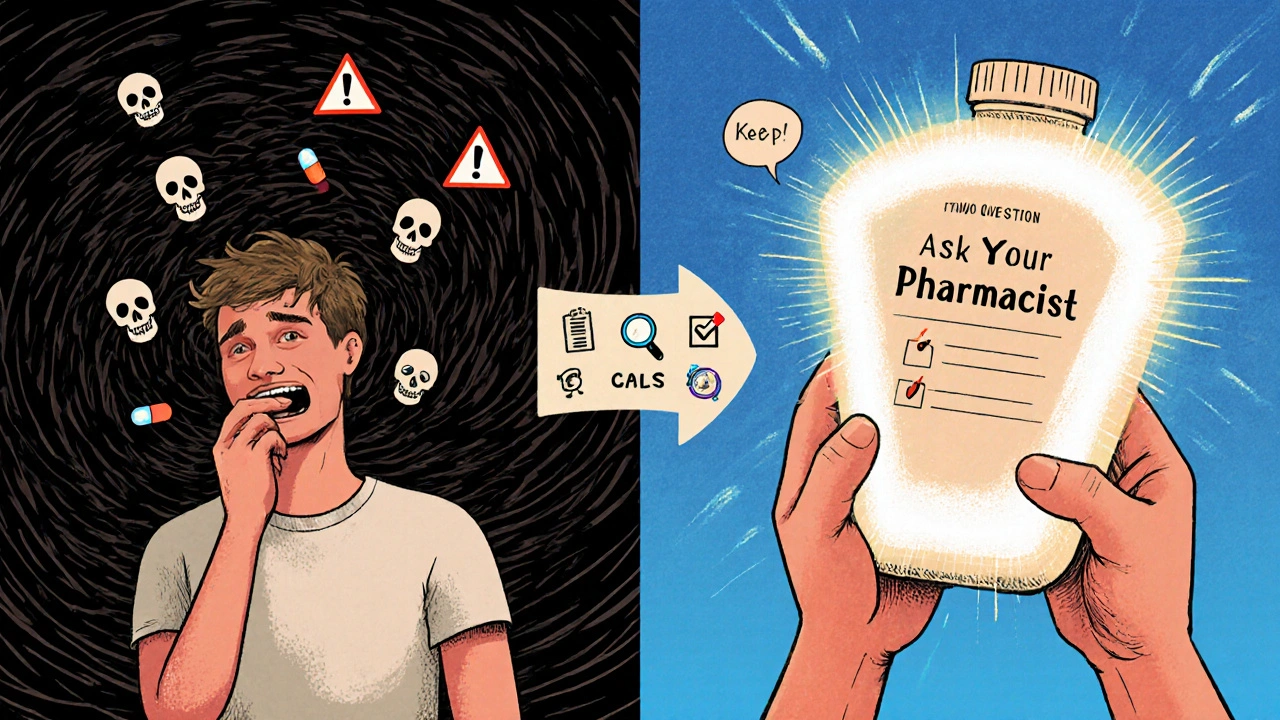
Ask for Help - Don’t Guess
You don’t have to figure this out alone. Pharmacists are trained to explain labels. In fact, 83% of people who used Drugs.com’s “Ask a Pharmacist” feature said they finally understood their warnings after talking to someone.When you pick up a new prescription, say: “Can you walk me through the interaction warnings on this?” Bring all your meds - prescriptions, OTCs, supplements - in a bag. Pharmacists catch interactions in 22% of cases during these reviews.
If the label is too small to read, ask for a large-print version. If the language is confusing, ask for a plain-English explanation. No one should be expected to decode medical jargon on their own.
Special Cases: Kids and Seniors
Children’s medications are especially risky. The CDC found that 67% of dosing errors happen because parents misread labels. Always use the measuring tool that comes with the bottle - never a kitchen spoon. Read the label twice: once for the active ingredient, once for the dose.Seniors are the most vulnerable group. Two out of three adults over 65 take five or more medications daily. That’s a recipe for interaction chaos. The FDA is testing QR codes on bottles that link to updated interaction info. In 2025, pilot programs are launching in 150 pharmacies. For now, stick to the basics: keep a list, talk to your pharmacist, and never assume a new pill is safe just because it’s “natural” or “over-the-counter.”
What to Do If You Miss a Warning
If you realize you’ve been taking two drugs that shouldn’t be mixed - don’t panic. Don’t stop cold turkey unless told to. Call your doctor or pharmacist immediately. Say: “I just saw that [Drug A] and [Drug B] can interact. What should I do?” They’ll tell you whether to adjust the dose, switch one, or monitor for symptoms.Watch for signs like unusual bruising, dizziness, nausea, confusion, or irregular heartbeat. These can be early signs of a dangerous interaction. Don’t wait for it to get worse.
Make It Routine
Reading your label shouldn’t be a one-time thing. Every time you get a new prescription, or your dose changes, check the label again. Medications change. Your body changes. What was safe last month might not be safe now.Set a reminder on your phone: “Check meds label - every 30 days.” It takes less than two minutes per bottle. That’s less time than it takes to scroll through social media. But it could mean the difference between staying healthy and ending up in the ER.
Can I rely on my pharmacy’s warning sticker instead of reading the label?
No. Pharmacy warning stickers are helpful, but they’re summaries - not full disclosures. They might say “Avoid alcohol” but miss interactions with other drugs or supplements. Always read the full label. The sticker is a reminder, not a replacement.
What if the label says “interaction possible” but doesn’t say what to do?
That’s a red flag. Under FDA’s 2024 rules, every clinically significant interaction must include clear instructions. If it doesn’t, call your pharmacist. It’s either outdated labeling or a missing warning. Either way, you need clarification before taking the drug.
Do generic drugs have the same interaction warnings as brand names?
Yes. Generic drugs contain the same active ingredient as brand names, so their interaction risks are identical. The label may look different, but the warnings are legally required to match. Don’t assume generics are safer or less risky.
Can food or drinks interact with my medication?
Absolutely. Grapefruit juice can make some cholesterol and blood pressure drugs dangerously strong. Alcohol can increase drowsiness from painkillers or antidepressants. Dairy can block absorption of antibiotics like tetracycline. Always check the label for food or drink warnings - they’re part of the interaction info.
How often should I update my medication list?
Every time you start, stop, or change a dose - even for something small like a vitamin. Keep a printed or digital list and update it weekly. Share it with every doctor and pharmacist you see. It’s the single most effective way to prevent interactions.









Sakthi s
14 Nov 2025 at 17:28This is the kind of info every single person on meds needs to see. Simple, clear, life-saving.