Military Medication Heat Impact Calculator
Medication Impact Calculator
Impact Assessment
When a soldier needs an epinephrine auto-injector during a heatwave in the Middle East, it doesn’t matter if the medicine was made perfectly in a lab. If it was stored at 50°C for 12 hours on a truck, it might as well be water. This isn’t science fiction-it’s daily reality in military operations. Medications that save lives on the home front can fail silently in the field, not because of poor manufacturing, but because of heat, broken refrigeration, and delayed access. The U.S. military spends millions every year to keep drugs cold, but the system is under constant stress-and the cost isn’t just financial. It’s measured in lives at risk.
Why Heat Destroys Military Medications
Most people think medicine stays good as long as it’s in the bottle. That’s true in a cool pharmacy. Not in a desert. Vaccines for anthrax, rabies, and even COVID-19 are designed to work within a narrow temperature range: 2°C to 8°C. Go above that, even for a few hours, and potency drops. The U.S. Army Medical Materiel Center-Southwest Asia found that in extreme heat, some vaccines lose up to 50% of their effectiveness in just 30 minutes. That’s not a small risk. That’s mission failure. Antibiotics aren’t immune either. A 2024 study from Walter Reed National Military Medical Center showed that 18% of antibiotics shipped to Middle Eastern bases lost effectiveness after being exposed to temperatures over 30°C for more than two days. Insulin, epinephrine, and other life-saving drugs are especially vulnerable. One medic from Camp Arifjan reported 147 temperature excursions in a single year-most happened during the final leg of delivery, when supplies were moved by vehicle across open desert with no cooling. The problem isn’t just storage. It’s the environment. Climate Central data shows that deployment zones like Kuwait and Iraq had 23 more days above 40°C in 2024 than in 2020. That’s not a trend-it’s a threat. The military’s current cold chain was built for 2010 conditions, not 2025. And it’s breaking.How Medications Are Supposed to Be Stored
The military follows strict rules laid out in the Cold Chain Management Principles (April 2025 update) and CENTCOM’s CCOP-03 policy. Refrigerated meds must stay between 2°C and 8°C. Frozen ones need -50°C to -15°C. Ultra-cold vaccines, like some mRNA shots, require -90°C to -60°C. Room-temperature meds? Still have to stay between 15°C and 30°C. No exceptions. Every storage unit-whether it’s a fridge in a forward operating base or a shipping container on a cargo plane-must have two temperature monitors: one digital, one physical. Both are checked twice a day, every day. No shortcuts. If the temperature spikes above 8°C, the log must be filled out immediately, the cause identified, and the meds quarantined. In civilian pharmacies, a brief warm spell might be written off. In the military, it’s a reportable incident. Ships and trucks carrying meds must use insulated boxes with gel packs and Temp-Tale devices-small digital loggers that record every temperature change. These systems can hold 2°C-8°C for up to 72 hours, even in 40°C heat. But they’re not foolproof. When the generator fails, when the truck breaks down, when the medics have to move fast-those systems can’t always keep up.
The Real-World Breakdowns
A 2024 survey of 327 deployed medics found that 68% had seen medication compromised by heat. In 83% of those cases, it was insulin or epinephrine. One Reddit post from a medic named SpecOpsPharmD described how his unit modified MRE coolers with phase-change materials to keep insulin cold for 12 hours in 45°C heat. That’s not standard procedure. That’s improvisation born of necessity. The biggest failures happen during last-mile delivery. Forward operating bases often get their meds via convoy. If the convoy is delayed, if the vehicle’s AC dies, if the driver has to take a dirt road to avoid IEDs-temperature control vanishes. In 2023, 72% of all temperature excursions reported by Camp Arifjan happened during these final transfers. The meds arrived warm. The soldiers got weaker protection. And then there’s the paperwork. CENTCOM requires medics to manually check and log temperatures every six hours if they don’t have remote monitoring. That’s 45 minutes a day, every day, spent not treating patients, not training, not sleeping-just recording numbers. A 2024 Army Medical Logistics Command report found 57% of medics said this task interfered with their primary duties. That’s not efficiency. That’s a system designed for control, not care.Access Delays in Extreme Heat
It’s not enough to have the right meds. You have to get them to the soldier in time. In temperate conditions, medics can administer emergency drugs in about 12 minutes. In heat above 35°C, that time jumps to 47 minutes. Why? Because the gear is heavier. The uniforms are hotter. The medics are exhausted. The vehicles are slower. The chain of command gets tangled. Epinephrine auto-injectors are a perfect example. They’re designed to work at body temperature. But if they’ve been sitting in a hot vehicle, the chemical buffer changes. Studies from the Iowa Harm Reduction Coalition show that while the drug still works at 70°C, the delivery mechanism becomes less reliable. The needle might not fire. The dose might be uneven. In a combat situation, that’s a death sentence. Soldiers carry their own epinephrine and insulin. But when they’re on patrol, in a Humvee, under fire, in 50°C heat-those meds are just as exposed as the ones in the field medics’ packs. There’s no refrigeration. No backup. No one checking the temperature log.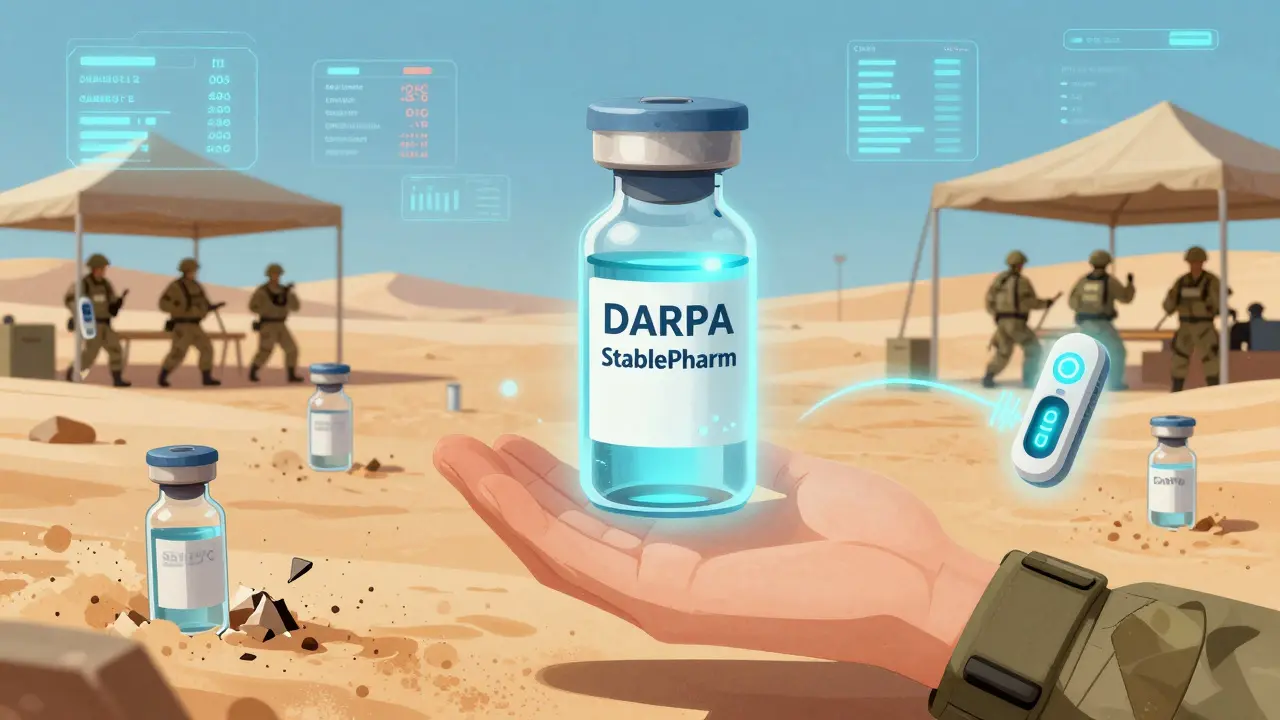
What’s Being Done to Fix It
The military isn’t ignoring the problem. It’s investing. By December 2023, every combatant command had adopted digital temperature monitoring systems. Paper logs are gone. Everything is tracked electronically. That alone cut medication waste by $2.3 million annually across CENTCOM theaters. New tech is coming. In March 2025, the Army tested AI-powered predictive models at Fort Bragg. The system analyzed weather, transport routes, and equipment status to forecast where temperature excursions were likely. It reduced those events by 22% in just a few months. The Defense Advanced Research Projects Agency (DARPA) is spending $28 million on StablePharm-a program to create drugs that stay effective at 65°C. Early results show some antibiotics now last twice as long in heat. That’s huge. If they can make insulin stable at 50°C, it could change everything. The military is also pushing for better packaging. By 2028, 75% of military pharmaceuticals are expected to have IoT sensors built into the vials or auto-injectors. That means real-time tracking-not just for the supply chain, but for the soldier carrying it.The Bigger Picture
This isn’t just about medicine. It’s about readiness. The RAND Corporation warned in 2024 that without major upgrades, medication efficacy in extreme heat could drop 15-20% by 2030. That means 60% of high-temperature deployments could see reduced protection against disease, slower recovery from injury, and higher rates of mission failure. The military’s cold chain is one of the most complex logistics systems on Earth. It moves vaccines across deserts, mountains, and oceans. But it’s still built on 20th-century assumptions. The world is hotter. The missions are longer. The threats are more unpredictable. The solution isn’t just better fridges. It’s better drugs. Better training. Better systems that don’t rely on soldiers to be part-time temperature loggers. It’s time to stop treating medication safety like a paperwork problem-and start treating it like the life-or-death mission it is.Can military vaccines still work after being exposed to high heat?
Some can, but not reliably. Studies show vaccines like those for anthrax, rabies, and COVID-19 can lose up to 50% of their potency in just 30 minutes when exposed to temperatures above 40°C. Even if the vial looks fine, the immune response it triggers may be too weak to protect soldiers. The military discards any vaccine with a documented temperature excursion outside 2°C-8°C, because the risk isn’t worth it.
Why don’t military medics just use regular coolers?
Standard coolers can’t maintain the precise 2°C-8°C range needed for vaccines and insulin. They also don’t have digital temperature logs, which are mandatory under military policy. Some medics improvise by modifying MRE coolers with phase-change materials, but those aren’t approved or tested for safety. The military uses insulated shipping boxes with certified gel packs and Temp-Tale devices because they’re the only ones that meet the required standards.
What happens if a temperature excursion isn’t reported?
It’s a serious violation. Every temperature excursion must be documented with root cause analysis and corrective actions. Unreported events can lead to disciplinary action, loss of medical clearance, and even mission suspension. More importantly, undetected degraded meds put entire units at risk. In Operation Inherent Resolve, units with unreported excursions had 12% lower seroconversion rates-meaning more soldiers were unprotected against disease.
Are there any medications that don’t need refrigeration in the field?
Yes. Some antibiotics, painkillers, and antihistamines are stable at room temperature and don’t require cold chain management. But the most critical drugs-vaccines, insulin, epinephrine, and certain antivirals-do. The military prioritizes these for cold chain protection because their failure has the highest consequence. Always check the manufacturer’s label, even if it’s been in the field for months.
How do soldiers carry emergency meds like epinephrine in hot environments?
Soldiers carry auto-injectors in their personal gear, usually in a pocket or chest rig. There’s no refrigeration. The military assumes these will be used quickly, within hours, so short-term heat exposure is accepted as a risk. But research shows even brief exposure to 50°C can alter the drug’s delivery mechanism. The Army is testing new heat-stable auto-injectors, but none are fielded yet. For now, the rule is: use it if needed, even if it’s been hot-but know the risk.









Tim Goodfellow
20 Dec 2025 at 07:23This is wild. I never realized how much of a gamble it is just to keep a life-saving shot from turning into fancy saline. Picture this: your epinephrine’s been baking in a truck like a soda can at a BBQ, and then you need it to save a buddy’s life. The needle might not even fire. That’s not a system failure-it’s a betrayal. And they’re still using paper logs? In 2025? Come on.
They’re spending millions on drones and stealth tech but can’t fix the damn fridge? I’d rather see half that budget go to heat-stable meds than another stealth bomber that flies over a desert no one cares about.
Also-phase-change materials in MRE coolers? That’s the kind of genius that happens when you’re out there with nothing but duct tape and grit. Someone’s gotta make this official. Stop glorifying improvisation. Fix the damn system.