What Happens to Your Liver When You Stop Drinking?
When you stop drinking after long-term heavy use, your liver doesn’t just relax-it goes into crisis mode. For years, it’s been working overtime to break down alcohol, turning ethanol into toxic acetaldehyde and then into harmless acetate. But when alcohol suddenly disappears, the liver’s metabolic pathways get thrown off balance. Blood flow shifts, enzymes go haywire, and inflammation spikes. This isn’t just discomfort-it’s a physiological storm that can actually make liver damage worse before it gets better.
Up to 32% of people who quit drinking see their liver enzymes (AST and ALT) rise sharply in the first week, even though they’ve stopped consuming alcohol. Why? Because the liver, already stressed from years of processing toxins, is now trying to repair itself while also dealing with the shock of withdrawal. This spike doesn’t mean you’re doing something wrong-it means your body is reacting. The key is managing this phase safely.
Why Medical Supervision Isn’t Optional
Trying to quit alcohol on your own, especially if you’ve been drinking heavily for months or years, is risky. About 5% of people going through withdrawal develop delirium tremens (DTs)-a life-threatening condition with seizures, hallucinations, and extreme confusion. Without medical help, the chance of surviving DTs drops dramatically.
Medically supervised detox cuts the risk of serious complications from 35% down to just 5%. Hospitals and specialized clinics use benzodiazepines like chlordiazepoxide to calm the nervous system and prevent seizures. These aren’t just sedatives-they’re lifesavers during withdrawal. Studies show they’re 85% effective at stopping seizures, compared to only 40% with symptom-triggered approaches.
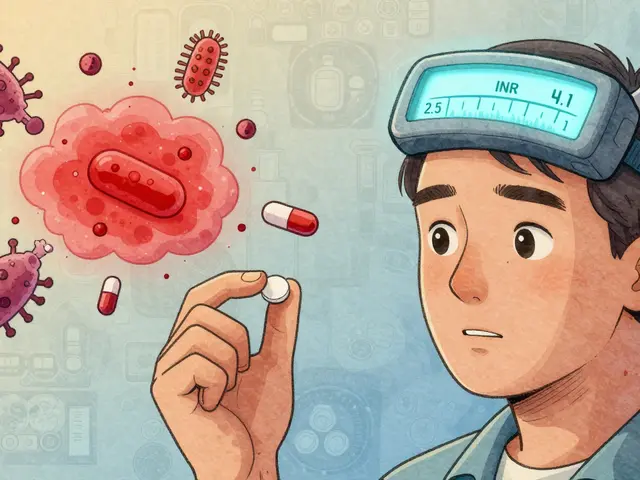
And it’s not just about seizures. Your liver is more vulnerable than ever right after quitting. Even a small dose of paracetamol (acetaminophen)-something many people take for headaches or fever-can cause severe liver injury during this time. One study found that people who took just 1-2 grams of paracetamol daily after quitting had the highest spikes in liver enzymes. That’s less than two standard painkiller tablets. You might think you’re helping yourself, but you’re putting your liver at risk.
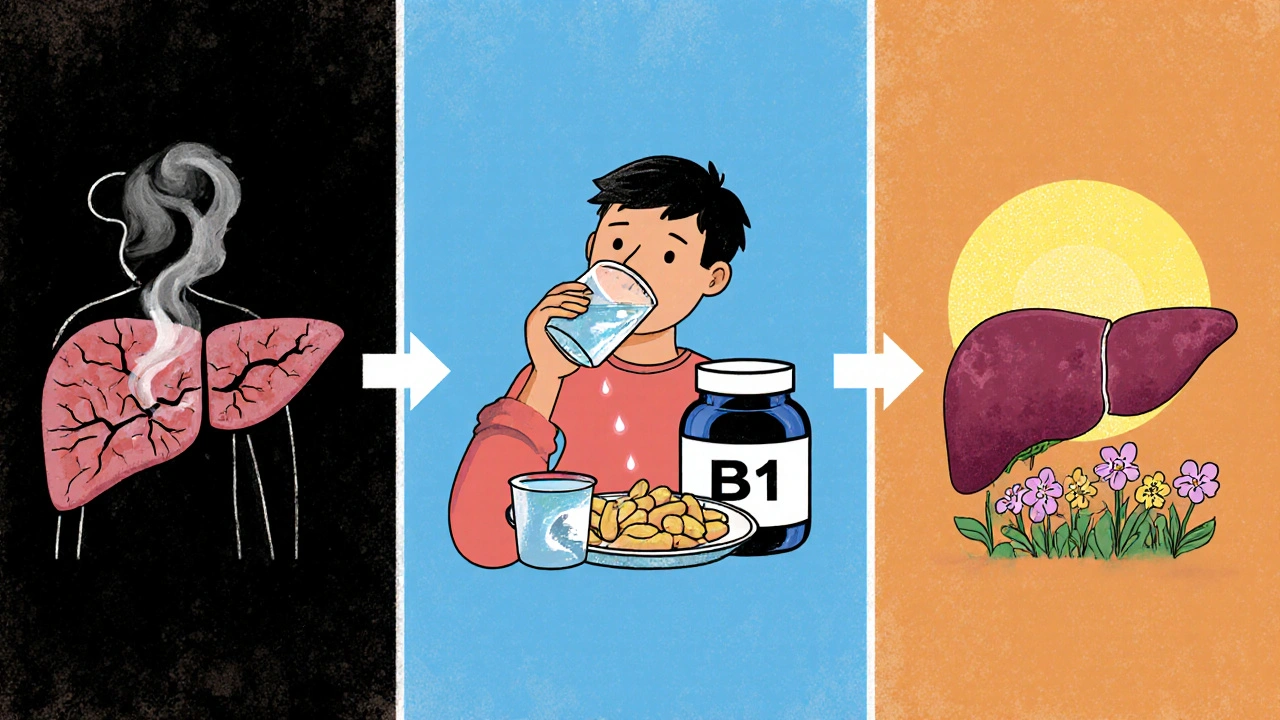
The Liver’s Amazing Ability to Heal
The good news? Your liver is one of the few organs that can regenerate. If you stop drinking and give it time, it can repair itself-even after years of damage. In mild cases of fatty liver disease, liver enzymes often return to normal within 7-14 days. After 4-8 weeks of complete abstinence, most people see clear improvements in liver function. And within 3-12 months, even those with moderate damage can show significant recovery.
But this only happens with total abstinence. There’s no such thing as "cutting back" if you want your liver to heal. The Cleveland Clinic says it plainly: if alcoholic hepatitis isn’t too far advanced, it can be reversed-by quitting alcohol. Those who don’t quit will keep moving toward cirrhosis and liver failure.
Don’t be fooled by myths. Some think drinking wine in moderation after a detox is safe. It’s not. Once your liver has been damaged by alcohol, even small amounts can restart the cycle of inflammation and scarring. For people with alcoholic hepatitis or cirrhosis, lifelong abstinence isn’t a suggestion-it’s the only path to survival.

What to Eat and Take During Detox
Your liver doesn’t heal in a vacuum. It needs fuel. And during withdrawal, your body is likely depleted of key nutrients from years of poor diet and alcohol’s interference with absorption.
Thiamine (vitamin B1) is critical. Without it, you risk Wernicke-Korsakoff syndrome-a neurological disorder that can cause memory loss, confusion, and even permanent brain damage. The NHS recommends 500mg of IV thiamine daily for the first 3-5 days of detox. After that, oral supplements are fine, but don’t skip it.
Protein intake matters too. Aim for 1.2-1.5 grams of protein per kilogram of body weight daily. That’s about 80-100 grams for a 70kg person. Lean meats, eggs, fish, beans, and dairy help rebuild liver cells. Low protein means slower healing and higher risk of complications.
N-acetylcysteine (NAC), an antioxidant, has been shown in clinical trials to reduce liver enzyme spikes by 30% during withdrawal. It’s not a magic cure, but it helps your liver fight oxidative stress. You can get it as a supplement, but talk to your doctor first-especially if you’re on other medications.
Hydration is non-negotiable. Alcohol dehydrates you, and dehydration makes withdrawal symptoms worse. Drink water, broth, and electrolyte drinks. Avoid sugary sodas-they add stress to your liver.
What to Avoid During Detox
There are silent killers during alcohol withdrawal that most people don’t know about.
- Paracetamol (acetaminophen): Even at normal doses, it’s dangerous during detox. Use ibuprofen or naproxen instead for pain, but only if your kidneys are okay.
- Other medications: Many antibiotics, antifungals, and antidepressants are processed by the liver. Tell every doctor you see that you’re in withdrawal-they need to adjust dosages.
- Energy drinks and caffeine: They raise heart rate and blood pressure, which are already elevated during withdrawal. Stick to herbal teas or water.
- Herbal "liver cleanses": Products like milk thistle or dandelion root sound harmless, but they’re not regulated. Some can interact with medications or even harm your liver further.
- Alcohol "tapering": Some people try to slowly reduce intake. But for those with moderate to severe dependence, this often leads to continued liver damage. If you’re dependent, go cold turkey-with medical help.
How Long Does Recovery Take?
There’s no one-size-fits-all timeline. It depends on how much you drank, how long, and how damaged your liver already was.
For mild fatty liver: 6 weeks of abstinence can lead to full recovery. Blood tests return to normal. Fat leaves the liver. You feel better.
For alcoholic hepatitis: 3-6 months of abstinence are needed to see major improvement. Some scarring may remain, but inflammation drops. Survival rates jump from 50% to 90% if you stop drinking.
For cirrhosis: The liver can’t fully reverse scarring, but stopping alcohol can stop progression. Many people live for decades with cirrhosis if they stay sober. The key is preventing complications like fluid buildup, bleeding, or liver cancer.
One study in Scientific Reports found that even after years of heavy drinking, 70% of people who stayed sober for a year showed measurable improvement in liver stiffness-a sign of reduced fibrosis.
What Comes After Detox?
Detox is just the first step. The real challenge is staying sober. Studies show 70% of people who complete detox relapse within six months if they don’t have ongoing support.
That’s why recovery programs, counseling, and peer groups like Alcoholics Anonymous are so important. They don’t just help you avoid alcohol-they help you rebuild your life. Stress, isolation, and trauma are big triggers. Addressing those is part of protecting your liver.
Some clinics now use telemedicine to follow up with patients after detox. This has improved long-term outcomes by 25% in rural areas where access to specialists is limited. But if your liver enzymes are still high after detox, telemedicine isn’t enough-you need in-person monitoring.
When to Seek Emergency Help
Not every symptom of withdrawal is normal. If you experience any of these, go to the hospital immediately:
- Seizures
- Hallucinations (seeing or hearing things that aren’t there)
- Severe confusion or disorientation
- High fever (over 38.5°C)
- Yellow skin or eyes (jaundice)
- Dark urine or pale stools
- Swelling in your abdomen or legs
These aren’t "just withdrawal symptoms." They’re signs your liver is failing or you’re developing a life-threatening condition.
Final Reality Check
Alcohol-related liver disease kills more people in the West than any other cause of liver failure. Eighty percent of liver toxicity deaths are linked to alcohol. And yet, only 10% of people with alcohol use disorder get the help they need.
Quitting isn’t easy. But your liver doesn’t care how hard it is-it only cares if you stop. It doesn’t need fancy treatments, expensive supplements, or miracle diets. It just needs you to stop drinking and give it time.
If you’re reading this, you’re already thinking about change. That’s the first step. The next one? Reach out. Talk to a doctor. Get checked. Don’t wait for symptoms to get worse. Your liver can heal-but only if you give it a real chance.
Can I detox from alcohol at home safely?
For people with mild alcohol use and no history of seizures or liver disease, home detox might be possible with close monitoring. But if you’ve been drinking heavily for more than a few months, or if you have any signs of liver damage (jaundice, swelling, fatigue), home detox is dangerous. Medical supervision reduces complications by 30% and prevents life-threatening events like delirium tremens. Don’t risk it.
How do I know if my liver is damaged from alcohol?
The only reliable way is through blood tests and imaging. Key markers include AST and ALT levels, with an AST:ALT ratio above 2:1 strongly suggesting alcohol-related damage. Low albumin, high INR, and elevated bilirubin also point to liver dysfunction. An ultrasound or FibroScan can show fat buildup or scarring. If you’ve been drinking heavily for years, get tested-even if you feel fine.
Is it safe to take painkillers during alcohol withdrawal?
Avoid paracetamol (acetaminophen) completely during withdrawal-it’s extremely hard on your liver when it’s already stressed. Ibuprofen or naproxen are safer for short-term use, but only if your kidneys are healthy. Always check with your doctor before taking any medication, even over-the-counter ones. Many drugs are processed by the liver and can cause serious harm during detox.
Will my liver recover if I quit drinking now?
Yes-if you stop completely and give it time. Even after years of heavy drinking, the liver can regenerate. Mild fatty liver can reverse in 6 weeks. Alcoholic hepatitis improves in 3-6 months. Cirrhosis can’t be undone, but stopping alcohol stops further damage and greatly improves survival. The key is abstinence. No exceptions.
How long should I wait before drinking again after detox?
If you’ve had alcohol-related liver damage, you should never drink again. Even small amounts can restart inflammation and scarring. For those with mild fatty liver and no other damage, some doctors may allow limited drinking after 6 weeks of abstinence-but only if liver tests are normal and you stick to NHS guidelines (14 units per week max). But the safest choice? Never drink again. Your liver will thank you.
Are there supplements that help liver recovery?
N-acetylcysteine (NAC) has shown promise in reducing liver enzyme spikes during withdrawal. Thiamine (B1) is essential to prevent brain damage. A balanced diet with adequate protein is more important than any supplement. Avoid herbal "liver cleanses"-they’re unregulated and can be harmful. Focus on real food, hydration, and medical guidance, not quick fixes.






Margo Utomo
18 Nov 2025 at 01:35I’ve seen so many people try to quit cold turkey and end up in the ER. Seriously, if you’re reading this and you’ve been drinking for years, just call a doctor. 🤝💊 Your liver doesn’t need a hero-it needs a plan. You got this!