Phenytoin-Warfarin Interaction Calculator
Monitor Your Interaction Risk
This tool estimates how phenytoin affects your INR and warfarin dose requirements. Based on article guidelines, this is the most reliable way to manage this dangerous interaction.
INR Timeline & Dosing Recommendations
INR Estimates
Recommended Warfarin Doses
When you take phenytoin and warfarin together, your body doesn’t just handle two drugs-it handles a chemical tug-of-war that can swing your blood clotting risk up or down in a matter of days. This isn’t a simple case of one drug making the other stronger or weaker. It’s a two-phase battle inside your liver and bloodstream, and if you’re not watching closely, it can lead to bleeding or clots-both dangerous, both preventable.
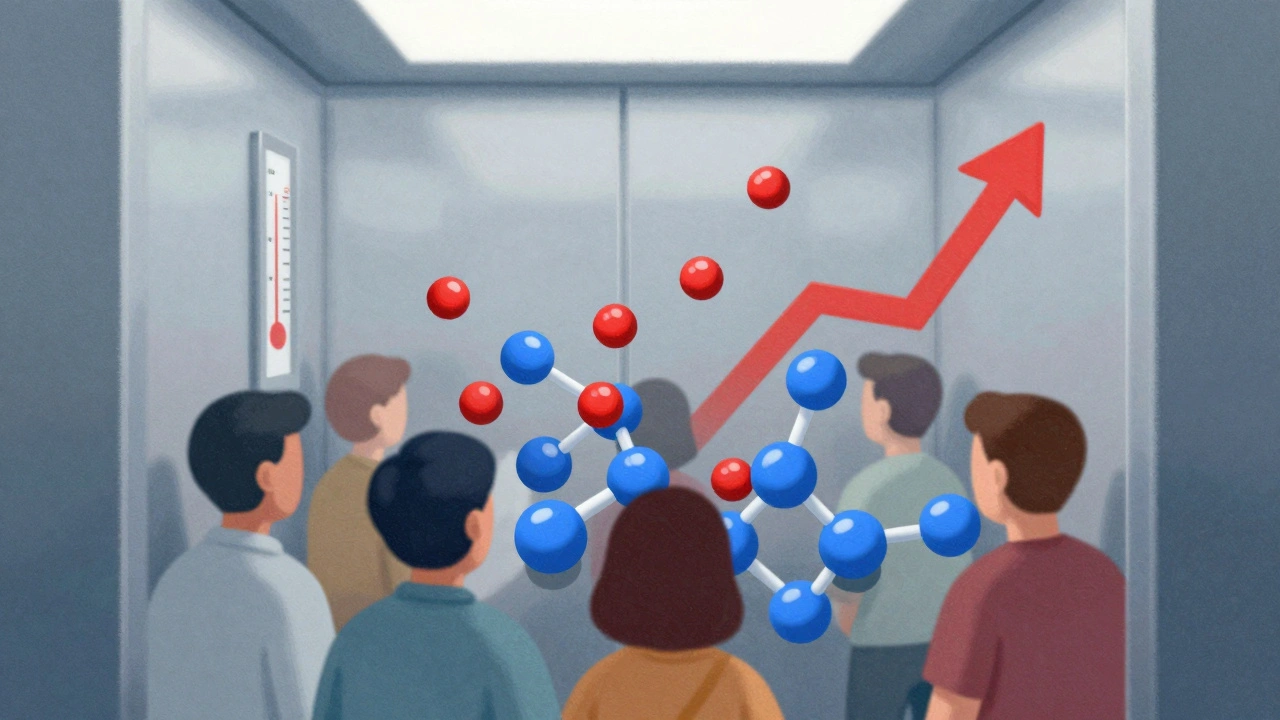
The First Wave: A Sudden Spike in INR
Within 24 to 72 hours of starting phenytoin, your INR can jump unexpectedly. That’s because phenytoin doesn’t just float in your blood-it clings tightly to albumin, the main protein that carries drugs around your body. Warfarin does the same. But phenytoin has a stronger grip. When it shows up, it kicks warfarin off those protein sites, freeing up more of the active, unbound warfarin in your bloodstream. That’s the part that actually thins your blood.Think of it like a crowded elevator. Warfarin was holding its spot. Then phenytoin pushes in, and suddenly, more warfarin is loose and active. Your INR rises. You might not feel anything, but your blood is now thinner than before. This spike is temporary. It usually settles back down in 3 to 5 days as your body redistributes the drugs. But if you don’t know this is coming, you might lower your warfarin dose thinking you’re over-anticoagulated-and that’s when things go wrong later.
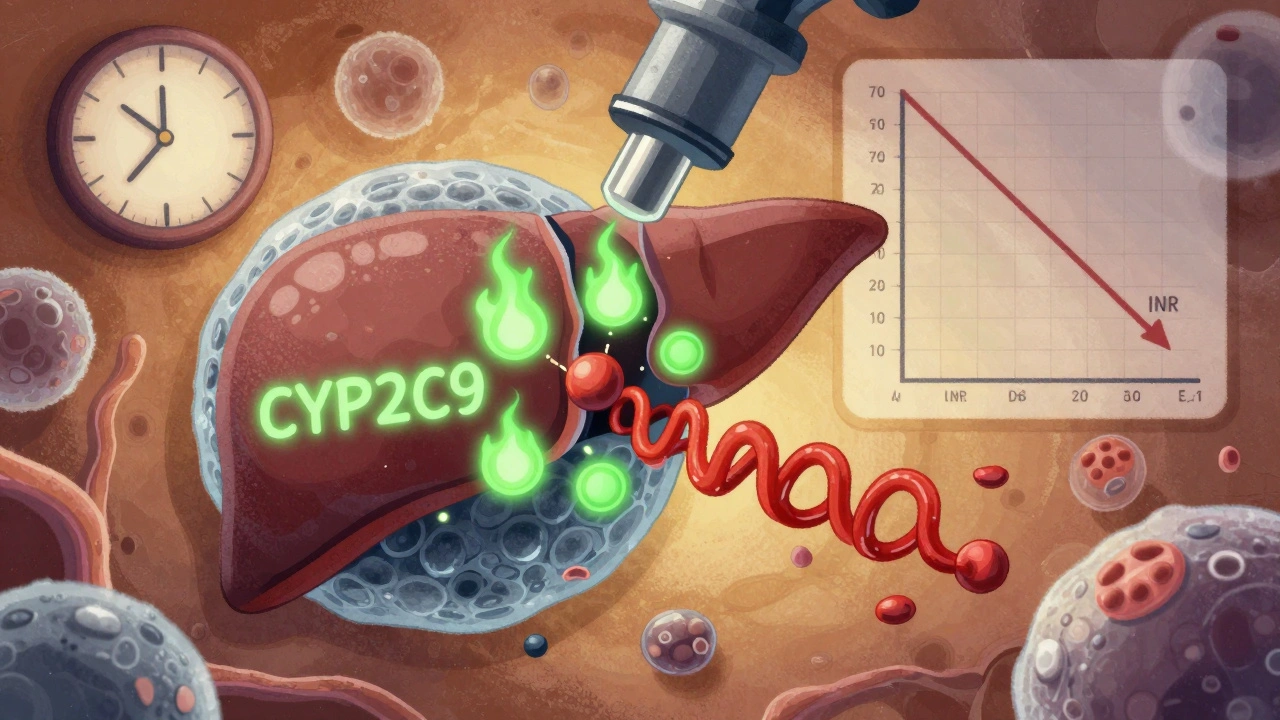
The Second Wave: The Slow Burn That Changes Everything
While the first spike fades, something quieter but far more powerful is building. Phenytoin turns on your liver’s drug-processing machinery. Specifically, it activates the pregnane X receptor, which tells your liver to produce more of the CYP2C9 and CYP3A4 enzymes. These are the same enzymes that break down warfarin, especially the more potent S-warfarin form.By day 7 to 10, your body is metabolizing warfarin twice as fast. That means you need way more of it to stay in the therapeutic range. Studies show patients on long-term phenytoin often require 2 to 5 times their original warfarin dose. One patient who was stable on 5 mg per day might suddenly need 20 mg to keep their INR at 2.5. If you don’t adjust, your INR drops. You’re no longer protected from clots. Atrial fibrillation, a mechanical heart valve, or deep vein thrombosis can turn deadly in days.
Why Some People Are Hit Harder Than Others
Not everyone reacts the same way. Genetics play a huge role. If you carry the CYP2C9*2 or CYP2C9*3 variant, your body naturally breaks down warfarin slower. When phenytoin kicks in, your liver scrambles to compensate-and the dose increase needed can be even larger. People with low albumin levels (common in older adults, liver disease, or malnutrition) also feel the protein displacement effect more strongly. A small drop in albumin from 4.0 to 3.2 g/dL can double the free warfarin fraction after phenytoin starts.Phenytoin’s own pharmacokinetics make it harder to predict. It doesn’t follow a straight line-small dose changes can cause big swings in blood levels. That’s why even if you get the warfarin dose right, a tiny bump in phenytoin (say, from 100 mg to 125 mg) can suddenly throw off your INR again.
What Happens When You Stop Phenytoin?
Many clinicians forget this part. Stopping phenytoin doesn’t just reverse the process-it reverses it slowly. The enzyme induction fades over 10 to 14 days. Your liver starts producing less CYP2C9. Warfarin builds back up. Your INR creeps up. If you don’t reduce your warfarin dose during this time, you risk serious bleeding.Experts recommend cutting your warfarin dose by 25% to 50% once phenytoin is stopped. But you can’t do it all at once. Monitor INR every 2 to 3 days for two weeks. Don’t assume you’re safe just because you stopped the drug. The danger is silent. No symptoms. Just a rising INR.
What About Other Antiepileptics?
You don’t have to use phenytoin. If you’re on warfarin and need an antiepileptic, there are better choices. Levetiracetam, gabapentin, and pregabalin don’t induce liver enzymes. They don’t displace warfarin. They don’t mess with INR. In fact, guidelines now recommend these as first-line options for patients on anticoagulants.Phenytoin is still used-especially in emergency settings like status epilepticus, or where newer drugs aren’t available. But if you’re planning long-term therapy, switching away from phenytoin can eliminate this entire risk. It’s not just safer-it’s simpler. Fewer blood tests. Fewer hospital visits. Fewer scares.
DOACs: The Alternative That Doesn’t Solve Everything
Direct oral anticoagulants (DOACs) like apixaban and rivaroxaban were supposed to make warfarin interactions a thing of the past. But here’s the catch: phenytoin also induces the enzymes that break down DOACs. So if you’re on phenytoin, most DOACs become ineffective. Their levels drop so low they can’t prevent clots. That’s why, for patients with mechanical heart valves or certain clotting disorders, warfarin is still the only option-even with phenytoin in the mix.This creates a narrow but critical space where the phenytoin-warfarin interaction isn’t just important-it’s unavoidable. You’re stuck managing it, not avoiding it.
How to Manage This Interaction in Real Life
Here’s what actually works in clinics:- Before starting phenytoin: Check your baseline INR. Know your current warfarin dose.
- Days 1-5: Check INR every 2 to 3 days. Expect a rise. Don’t reduce warfarin yet.
- Days 7-14: Watch for the INR to fall. This is when you’ll need to increase warfarin-often dramatically.
- After stabilization: Keep checking INR weekly for at least a month. Then, every 2 to 4 weeks if stable.
- If stopping phenytoin: Start reducing warfarin by 25% after 3 days. Monitor INR every 2-3 days for 14 days.
Don’t guess. Don’t rely on formulas. Don’t use the same dose you used for someone else. Every patient is different. The only reliable tool is the INR test.
What You Should Never Do
- Don’t increase warfarin right away when phenytoin starts. You’ll overshoot when the enzyme induction hits.
- Don’t assume a normal INR means you’re safe. It could be a temporary dip before the real drop.
- Don’t ignore symptoms like bruising, nosebleeds, or dark stools. They’re not always obvious.
- Don’t forget to tell every new doctor you’re on both drugs. Pharmacists, dentists, ER staff-they all need to know.
This interaction is one of the most dangerous in clinical practice. It’s not rare. It’s not theoretical. It’s happening right now in hospitals and homes across the country. And it’s preventable-if you know what to look for and when to act.
Can phenytoin cause bleeding when taken with warfarin?
Yes, but not directly. Phenytoin displaces warfarin from proteins in the first few days, increasing the amount of active warfarin in your blood. This can raise your INR and increase bleeding risk. The effect is temporary, but it’s real. That’s why INR must be checked within 72 hours of starting phenytoin.
How long does it take for phenytoin to affect warfarin levels?
There are two phases. The protein-binding effect starts within 24-72 hours and lasts 3-5 days. The enzyme-induction effect takes 7-10 days to fully develop and can last as long as phenytoin is taken. This is why monitoring must continue for weeks, not days.
Should I stop phenytoin if I’m on warfarin?
Not unless your doctor recommends it. Phenytoin is often necessary for seizure control. The goal isn’t to stop it-it’s to manage the interaction. Switching to a safer antiepileptic like levetiracetam is an option, but only if your seizures can be controlled without phenytoin. Never stop either drug without medical supervision.
Do DOACs work with phenytoin?
Most DOACs don’t work well with phenytoin. Phenytoin induces enzymes that break down apixaban, rivaroxaban, and dabigatran, lowering their levels to ineffective ranges. For patients with mechanical heart valves or certain clotting disorders, warfarin remains the only viable oral anticoagulant when phenytoin is needed.
What’s the best way to monitor this interaction?
Frequent INR testing is the only reliable method. Check INR every 2-3 days for the first 2 weeks after starting or stopping phenytoin. Once stable, weekly checks are usually sufficient. Point-of-care INR devices make this easier at home. Never rely on symptoms or guesswork.
If you’re on both drugs, your biggest tool isn’t a pill-it’s the INR machine. Stay consistent with testing. Keep your care team informed. And remember: this interaction is complex, but it’s not a mystery. It’s a pattern. Learn it. Track it. Manage it.






Geraldine Trainer-Cooper
6 Dec 2025 at 14:20Phenytoin and warfarin are basically two exes fighting over the same couch and somehow you're the one getting kicked out every time