Switching from a brand-name drug to a generic version can save you hundreds - sometimes thousands - of dollars a year. But how do you know if a generic is even available for your prescription? And more importantly, is it safe and effective? You don’t need a pharmacy degree to figure this out. Here’s how to check, step by step, using tools you already have access to.
Understand What Makes a Generic Medication Valid
A generic drug isn’t just a cheaper copy. It has to meet strict standards set by the FDA. For a generic to be approved, it must contain the same active ingredient, in the same strength, and delivered the same way (pill, injection, inhaler, etc.) as the brand-name version. It also has to be bioequivalent - meaning your body absorbs it at the same rate and to the same extent as the brand. The FDA requires generics to perform within 80-125% of the brand’s absorption levels. That’s not a guess. It’s tested in clinical trials.The FDA keeps a public list called the Orange Book, which rates every approved drug by therapeutic equivalence. You’ll see codes like AB, BX, or A. An AB rating means the generic is considered fully interchangeable with the brand. A BX rating means there are known issues - maybe the drug has a narrow therapeutic window, like warfarin or levothyroxine - and your doctor needs to approve any switch. Don’t assume all generics are the same. Check the rating.
Ask Your Pharmacist First - It’s the Fastest Way
Your pharmacist is your best ally. They have real-time access to formulary databases like Medi-Span and First Databank that tell them exactly which generics are approved, covered by your insurance, and in stock. In a 2022 JAMA study, pharmacists correctly identified generic alternatives 98.7% of the time.When you pick up your prescription, don’t just say, “Do you have a generic?” Say: “Is there a therapeutically equivalent generic available for this medication?” That phrasing makes it clear you’re asking about FDA-approved substitution, not just any cheaper pill.
Major pharmacy chains like CVS, Walgreens, and Rite Aid have automated systems that flag generic options at checkout. Over 90% of prescriptions filled at these locations are generics - and most of them are chosen automatically. But if you’re not asked, ask. It only takes 30 seconds. One person in Leeds saved £840 a year just by asking about their blood pressure medication.
Use the FDA’s Drugs@FDA Database
If you want to check on your own, go to the FDA’s Drugs@FDA website. It’s free, official, and updated daily. Search by the brand name - for example, “Lipitor.”Once you find the brand, look under “Therapeutic Equivalence Code.” If it says “AB,” then generic versions are approved and interchangeable. If it says “BX,” proceed with caution. The site also lists all approved generic manufacturers and their NDC codes - those 11-digit numbers on the pill bottle that help pharmacies track exact products.
This method takes 8-12 minutes the first time. But once you know how, it’s faster than calling your doctor. The FDA launched a simplified version of this tool in October 2023, designed specifically for patients. It’s no longer buried in jargon.

Check Your Insurance Plan’s Formulary
Your Medicare Part D or private insurance plan decides which drugs are covered - and which generics they prefer. Plans often have tiers: generics are usually Tier 1 (lowest cost), while brand-name drugs might be Tier 3 or 4.If you’re on Medicare, use the Medicare Plan Finder. It’s updated every October 15. Type in your medication, your zip code, and your plan. It will show you exactly which generics are covered, how much you’ll pay, and whether prior authorization is needed.
Many private insurers have similar tools on their websites. Log in to your member portal and search your prescription. You might be surprised how much cheaper the generic is - even after your copay.
Use GoodRx - But Don’t Rely on It Alone
GoodRx is popular because it shows cash prices for both brand and generic versions at nearby pharmacies. It’s great for comparing costs. But here’s the catch: GoodRx doesn’t tell you if a generic is therapeutically equivalent. It might show you a generic that’s cheaper - but if it’s rated BX, your doctor may not approve it.Use GoodRx to find price options, then cross-check the generic name with the FDA’s Orange Book. Don’t assume low price = safe swap. One user in Manchester switched to a generic based on GoodRx pricing - only to find out later it was BX-rated and caused unstable thyroid levels.
Watch Out for Common Pitfalls
There are a few traps to avoid:- Similar-sounding names: Zyrtec (antihistamine) vs. Zyprexa (antipsychotic). A mix-up can be dangerous. Always confirm the active ingredient - not just the brand name.
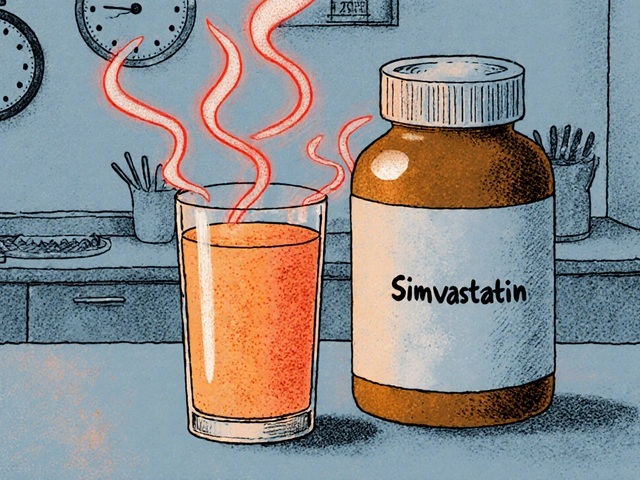
- Narrow therapeutic index drugs: Warfarin, lithium, levothyroxine, and some seizure meds are sensitive. Even small differences in how a generic is absorbed can cause side effects. Talk to your doctor before switching.
- Automatic substitution: Some plans switch your drug without telling you. Check your pharmacy receipt. If the name changed and you weren’t warned, call your doctor.
- Supply shortages: Sometimes, even the generic is unavailable. Check the ASHP Drug Shortages Database. As of November 2023, over 280 drugs were in short supply - including some generics.
When You Can’t Get a Generic
About 10% of medications still don’t have generic versions. Why? Patents. Brand-name companies hold exclusive rights for up to 17 years from patent filing - sometimes longer with extensions. Newer biologic drugs (like Humira or Enbrel) are especially slow to have generics. These are called biosimilars, and only 38 have been approved as of late 2023.If your drug has no generic, ask your doctor if there’s another brand-name drug in the same class that does. For example, if your brand-name statin has no generic, maybe a different statin does. Or ask if a mail-order pharmacy can get it cheaper. Sometimes, buying a 90-day supply reduces your per-pill cost significantly.
What to Do If Your Doctor Refuses
Some doctors are hesitant to switch to generics - especially for complex conditions. They might say, “I’ve always prescribed this brand.” But the science says otherwise. The FDA approves generics after rigorous testing. In fact, 90% of U.S. prescriptions are filled with generics.If your doctor refuses, ask why. Is it because of the drug’s therapeutic rating? Is it because of your medical history? If they say, “I just prefer the brand,” ask for evidence. You can bring up the FDA’s Orange Book or a study from JAMA or NEJM. Most doctors will reconsider when they see the data.
If they still won’t budge, you can request a prior authorization form from your insurance. Sometimes, insurers will approve the brand if you prove the generic didn’t work - but only after you’ve tried the generic first.
Bottom Line: You Have Power
You don’t have to pay full price for a brand-name drug unless you have to. Generic medications are safe, effective, and legally approved. The system is designed to help you save money - but you have to ask.Next time you get a prescription, do this:
- Ask your pharmacist: “Is there an AB-rated generic available?”
- Check the FDA’s Drugs@FDA website to confirm the rating.
- Log into your insurance portal to see your out-of-pocket cost for the generic.
- If the cost is still high, ask your doctor if another drug in the same class has a cheaper generic.
That’s it. Five minutes. One conversation. Potentially hundreds saved.
Can I switch from a brand-name drug to a generic without asking my doctor?
In most cases, yes - but only if the generic is rated AB by the FDA and your insurance allows substitution. Pharmacists can legally switch your prescription to an AB-rated generic unless your doctor specifically wrote “Dispense as Written” or “Do Not Substitute” on the prescription. If the generic is BX-rated, your doctor must approve the change. Always check your receipt to confirm what you received.
Are generic medications as effective as brand-name drugs?
Yes, for the vast majority of drugs. The FDA requires generics to have the same active ingredient, strength, and bioequivalence as the brand. Studies show they work just as well in treating conditions like high blood pressure, cholesterol, depression, and diabetes. The only exceptions are drugs with a narrow therapeutic index - like warfarin or levothyroxine - where tiny changes in absorption can matter. For those, your doctor may recommend sticking with one brand or generic.
Why are generic drugs so much cheaper?
Generic manufacturers don’t have to repeat expensive clinical trials. They only need to prove their version is bioequivalent to the brand. That cuts development costs by up to 90%. They also don’t spend millions on advertising. The FDA estimates generics save the U.S. healthcare system over $300 billion a year. In the UK, a 30-day supply of a brand-name statin might cost £120 - the generic version is often under £10.
What if my insurance won’t cover the generic?
That’s rare, but it can happen. Some plans have restrictions - like requiring you to try the brand first. If your generic isn’t covered, ask your pharmacist to submit a prior authorization request. You can also appeal to your insurer in writing. Many people successfully get coverage after explaining the cost burden. If all else fails, use GoodRx to find the lowest cash price - sometimes it’s cheaper than your insurance copay.
How do I know if a generic is actually the same as the brand?
Look up the drug in the FDA’s Drugs@FDA database. Search for the brand name, then check the “Therapeutic Equivalence Code.” If it’s AB, the generic is approved as interchangeable. You can also check the active ingredient - it must match exactly. The inactive ingredients (fillers, dyes) can differ, but they don’t affect how the drug works. If you’re unsure, ask your pharmacist to show you the FDA’s rating.







Vincent Soldja
3 Dec 2025 at 13:09Generic drugs work. FDA says so. End of story.