When doctors talk about idiopathic pulmonary fibrosis (IPF), two names dominate the conversation: Esbriet and its main competitor, Nintedanib. Both drugs slow the relentless decline in lung function, but they do it in very different ways and come with unique trade‑offs. This guide walks you through the science, the real‑world outcomes, and the practical considerations so you can see which option fits your situation best.
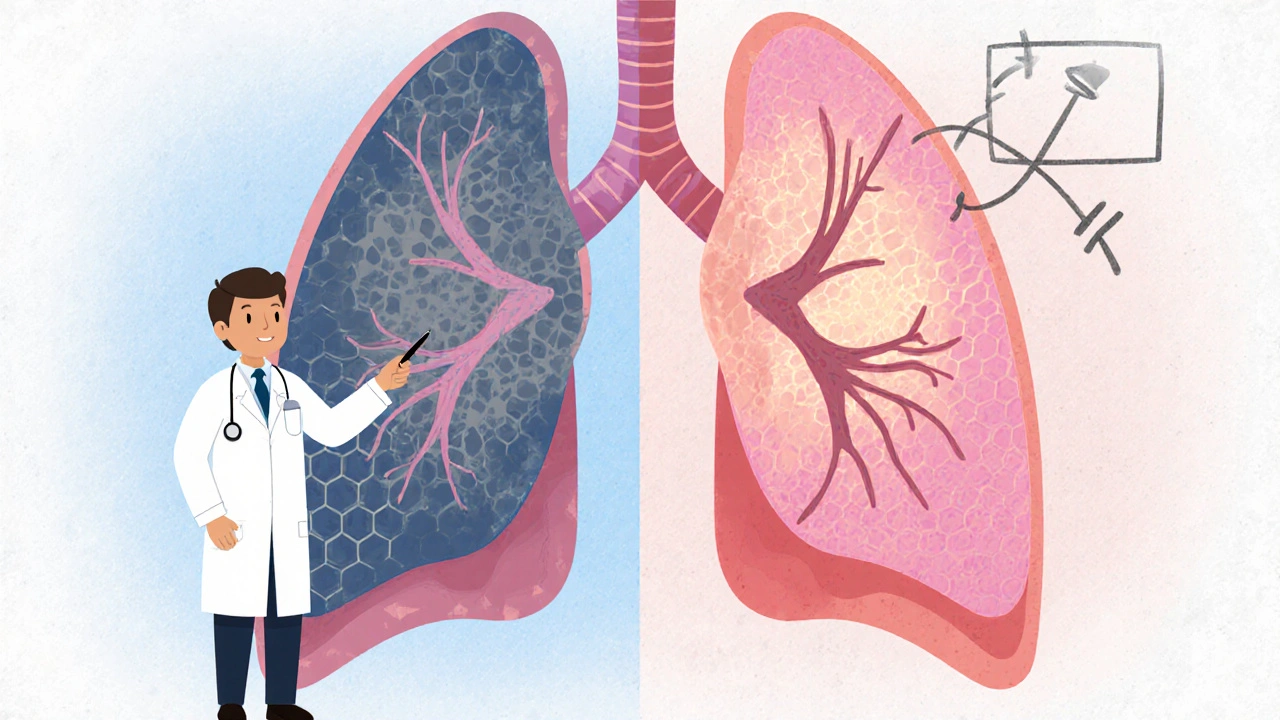
What is idiopathic pulmonary fibrosis?
IPF is a chronic, progressive lung disease where scar tissue builds up in the lungs for no obvious reason. The scarring, or fibrosis, stiffens the lung tissue, making it hard to breathe and reducing the forced vital capacity (FVC)-the amount of air you can exhale forcefully after a deep breath. Without treatment, most patients lose about 200 mL of FVC each year, leading to respiratory failure within 3‑5 years.
Esbriet (Pirfenidone): How it works
Esbriet (Pirfenidone) is a synthetic antifibrotic agent that modulates transforming growth factor‑beta (TGF‑β) and reduces fibroblast proliferation. It was first approved in the EU in 2011 and by the FDA in 2014.
- Mechanism: Inhibits collagen synthesis, dampens inflammatory cytokines, and blocks oxidative stress pathways.
- Dosing: 801 mg three times daily (with meals) after a 2‑week titration phase.
- Efficacy: In the CAPACITY trials, pirfenidone reduced the annual decline in FVC by about 50 % compared with placebo.
- Common side effects: Nausea, rash, photosensitivity, and loss of appetite.
- Cost (2025 US): Approximately $12,000‑$16,000 per year, depending on insurance coverage.
Because it must be taken with food, many patients report gastrointestinal upset, especially during the titration period. Sun protection is also a must due to photosensitivity.
Nintedanib (Ofev): The other FDA‑approved antifibrotic
Nintedanib is a tyrosine‑kinase inhibitor that targets multiple growth factor receptors involved in fibrosis. It received FDA approval in 2014 and EMA approval in 2015.
- Mechanism: Blocks receptors for platelet‑derived growth factor (PDGF), fibroblast growth factor (FGF), and vascular endothelial growth factor (VEGF).
- Dosing: 150 mg twice daily with food, no titration needed.
- Efficacy: In the INPULSIS trials, nintedanib lowered the annual FVC decline by roughly 45 % versus placebo.
- Common side effects: Diarrhea, liver enzyme elevations, nausea, and reduced appetite.
- Cost (2025 US): Roughly $13,500‑$18,000 per year.
Diarrhea is the most frequent adverse event, and many clinicians prescribe loperamide prophylactically. Liver function must be monitored every 4‑6 weeks during the first year.
Other therapies on the horizon
While Esbriet and Nintedanib dominate the market, several investigational agents are edging closer to approval:
- Pamrevlumab (FG‑3019): An anti‑connective tissue growth factor (CTGF) antibody that showed a 35 % slowdown in FVC loss in Phase 2 trials.
- Sildenafil: A phosphodiesterase‑5 inhibitor used off‑label for IPF‑related pulmonary hypertension; modest benefits in exercise capacity but no clear FVC advantage.
- Glucocorticoid pulse therapy: Historically used but now discouraged due to lack of efficacy and increased infection risk.
These options are typically considered for patients who cannot tolerate either pirfenidone or nintedanib, or who are enrolled in clinical trials.
Side‑by‑side comparison table
| Attribute | Esbriet (Pirfenidone) | Nintedanib |
|---|---|---|
| Year of first approval | 2011 (EU) / 2014 (US) | 2014 (US) / 2015 (EU) |
| Mechanism of action | Inhibits TGF‑β, reduces collagen synthesis | Broad tyrosine‑kinase inhibition (PDGF, FGF, VEGF) |
| Typical dosing schedule | 801 mg × 3 times daily (with meals) | 150 mg × 2 times daily (with food) |
| Annual FVC decline reduction | ~50 % vs placebo | ~45 % vs placebo |
| Most common adverse events | Nausea, photosensitivity, rash | Diarrhea, liver enzyme rise |
| Monitoring requirements | Liver enzymes, skin protection | Liver enzymes, weight, renal function |
| Typical yearly cost (US) | $12,000‑$16,000 | $13,500‑$18,000 |
| Special considerations | Must be taken with food; avoid sun | Prophylactic antidiarrheal meds often needed |
How to decide which drug is right for you
Choosing between Esbriet and Nintedanib isn’t just a numbers game. Real‑world decision‑making blends clinical data with personal lifestyle factors:
- Side‑effect tolerance: If you’re prone to gastrointestinal issues, pirfenidone’s nausea might be a deal‑breaker, whereas nintedanib’s diarrhea could be more manageable with medication.
- Meal patterns: Esbriet requires three meals a day for optimal absorption, so a busy schedule with irregular eating may favor nintedanib.
- Sun exposure: Outdoor workers should lean toward nintedanib to avoid photo‑sensitivity restrictions.
- Liver health: Both drugs affect liver enzymes, but nintedanib has a slightly higher incidence of transaminase elevation; baseline liver tests guide the choice.
- Insurance coverage: Formularies differ; one may be tier‑1 while the other is tier‑2, influencing out‑of‑pocket costs.
Discuss these points with a pulmonologist who can run a baseline assessment-spirometry, liver panel, and a quick review of your daily routine-to personalize the recommendation.
Managing side effects effectively
Even the best‑matched drug can cause trouble if side effects aren’t handled early. Here’s a quick cheat‑sheet:
- Nausea (Esbriet): Split the dose into smaller portions, take with high‑fat meals, and consider anti‑emetics like ondansetron for the first two weeks.
- Photosensitivity (Esbriet): Use SPF 50+ sunscreen, wear wide‑brimmed hats, and avoid peak UV hours.
- Diarrhea (Nintedanib): Begin loperamide 2 mg at the first sign, stay hydrated, and keep a low‑fiber diet during the first month.
- Liver enzyme rise (both): Check ALT/AST every 4 weeks for the first 6 months; pause treatment if levels exceed three times the upper limit of normal.
Most patients stay on therapy for years once side effects are under control, which is crucial because the benefit-slowing disease progression-only appears with continuous use.
Future outlook and ongoing research
Researchers are exploring combination therapy-using pirfenidone and nintedanib together-to see if additive benefits exist. Early Phase 2 data suggest a modest extra FVC preservation, but safety concerns (increased GI toxicity) keep the combo in trial phases. Gene‑editing approaches targeting fibroblast activation pathways are also on the horizon but remain experimental.
For now, the two approved drugs are your main weapons. Staying informed about trial enrollment opportunities can give access to cutting‑edge treatments before they hit the market.
Frequently Asked Questions
Can I switch between Esbriet and Nintedanib?
Yes. Most clinicians will implement a 2‑week washout period to clear the first drug, then start the new medication at the recommended dose. Monitoring liver enzymes during the transition is essential.
Are there any food interactions I should worry about?
Pirfenidone must be taken with food to improve absorption and reduce nausea. High‑fat meals are ideal. Nintedanib also requires food, but any balanced meal works; there’s no specific macronutrient requirement.
What happens if I miss a dose?
For pirfenidone, take the missed dose as soon as you remember if it’s within 6 hours; otherwise skip it and resume normal schedule. For nintedanib, skip missed doses and do not double‑dose.
Is lung transplantation an alternative to medication?
Transplant is a last‑resort option for end‑stage IPF when drug therapy can no longer preserve lung function. It offers a potential cure but comes with lifelong immunosuppression and limited donor availability.
How do I know if my treatment is working?
Pulmonary function tests (PFTs) measuring FVC every 3‑6 months are the standard metric. A slower decline than the historical baseline suggests the drug is effective.
Bottom line: both Esbriet and Nintedanib have solid evidence for slowing IPF, but the “best” drug hinges on your daily life, side‑effect profile, and insurance landscape. Armed with the data above, you can have a focused conversation with your healthcare team and pick the therapy that keeps you breathing easier for as long as possible.



Aimee White
23 Oct 2025 at 21:52It feels like Big Pharma is hiding a secret agenda behind the glossy brochures for Esbriet and Nintedanib.
The way they whisper about “side‑effect management” while pushing us to swallow endless pills is nothing short of a covert operation.
They want us dependent, glued to insurance formularies, while the real cure stays buried under layers of regulatory red tape.