Medication Neuropathy Risk Checker
Medication Assessment
Symptom Assessment
Your Risk Assessment
It starts small. A quiet tingling in your toes. Maybe your fingers feel like they’re wrapped in cotton. You shrug it off-medication neuropathy isn’t something most people think about until it’s too late. But these mild symptoms aren’t just annoying. They’re your body’s warning sign. And if you’re taking certain medications, ignoring them could mean permanent nerve damage.
What’s Really Going On When Your Feet Tingle?
Tingling and numbness from medications aren’t random. They’re signs of drug-induced peripheral neuropathy (DIPN), a condition where drugs damage the nerves outside your brain and spinal cord. These nerves control sensation in your hands and feet. When they get irritated or injured, you feel it as pins and needles, burning, or just… nothing at all. The pattern is classic: it starts in your toes or fingertips and creeps upward like a glove or stocking. That’s why doctors call it the “glove and stocking” distribution. It’s not just discomfort-it’s a red flag that nerve cells are being harmed. And here’s the thing: this isn’t rare. About 4% of all neuropathy cases come from medications. But if you’re on chemotherapy? That number jumps to 60%.Which Medications Are Most Likely to Cause This?
Not all drugs do this. But some are well-known offenders. The biggest culprits are chemotherapy agents. Oxaliplatin, used for colon cancer, causes tingling in up to 95% of patients during treatment. Paclitaxel, used for breast and lung cancer, affects 60-70%. Even after stopping, symptoms can keep getting worse for months. Then there’s isoniazid, an antibiotic for tuberculosis. It causes neuropathy in 10-20% of people on standard doses. Metronidazole, often prescribed for infections, can do the same after long-term use. Antiretrovirals like stavudine for HIV, and even some heart drugs like amiodarone, carry risks too. Statins? The evidence is shaky. Some people report numbness, but studies suggest it’s more likely coincidence than cause. Still, if you notice symptoms after starting a new drug-no matter how common it is-don’t assume it’s nothing.Why This Isn’t Just “Normal Side Effects”
Many patients are told, “It’s just a side effect,” and told to tough it out. But that’s dangerous advice. These symptoms aren’t like a headache or nausea. They’re early signals of nerve damage. And once nerves die, they don’t grow back easily. The good news? If caught early, DIPN can often be reversed. Studies show that 73% of people who stopped their medication at the first sign of tingling saw their symptoms improve or vanish within six months. But if you wait until your feet feel like they’re made of wood, or you can’t button your shirt? Recovery becomes much harder. Doctors use a grading system called CTCAE to measure severity. Grade 1 means mild-just tingling, no real interference with daily life. That’s the sweet spot for intervention. By Grade 3, you’re losing function. That’s when you might need to stop the drug completely.
How Doctors Spot It Before It’s Too Late
A good doctor doesn’t wait for you to complain. They check. Before starting high-risk drugs like cisplatin or bortezomib, they do a baseline neurological exam. They ask about sensation, balance, reflexes. Some use tools like the Total Neuropathy Score or the EORTC QLQ-CIPN20 questionnaire-standardized forms that track changes over time. New tech is helping too. The SudoScan device, approved by the FDA in 2021, measures how well your sweat glands respond. It can detect nerve damage before you even feel symptoms. That’s huge. It means we’re moving from waiting for pain to catching it before it starts. Still, only 35% of oncology clinics in the U.S. use these tools regularly. Community practices lag behind academic centers. That’s a gap. If your doctor isn’t monitoring you, ask. Don’t wait for them to bring it up.What You Can Do Right Now
If you’re on a medication linked to neuropathy, here’s what to do:- Check your feet and hands daily. Look for changes in color, swelling, or sores. Loss of sensation means you won’t feel cuts or blisters-those can turn into serious infections.
- Wear supportive shoes. Avoid walking barefoot. Even a small stone can cause damage you won’t feel.
- Keep your home well-lit and free of clutter. Falls are a real risk when your feet don’t feel the ground.
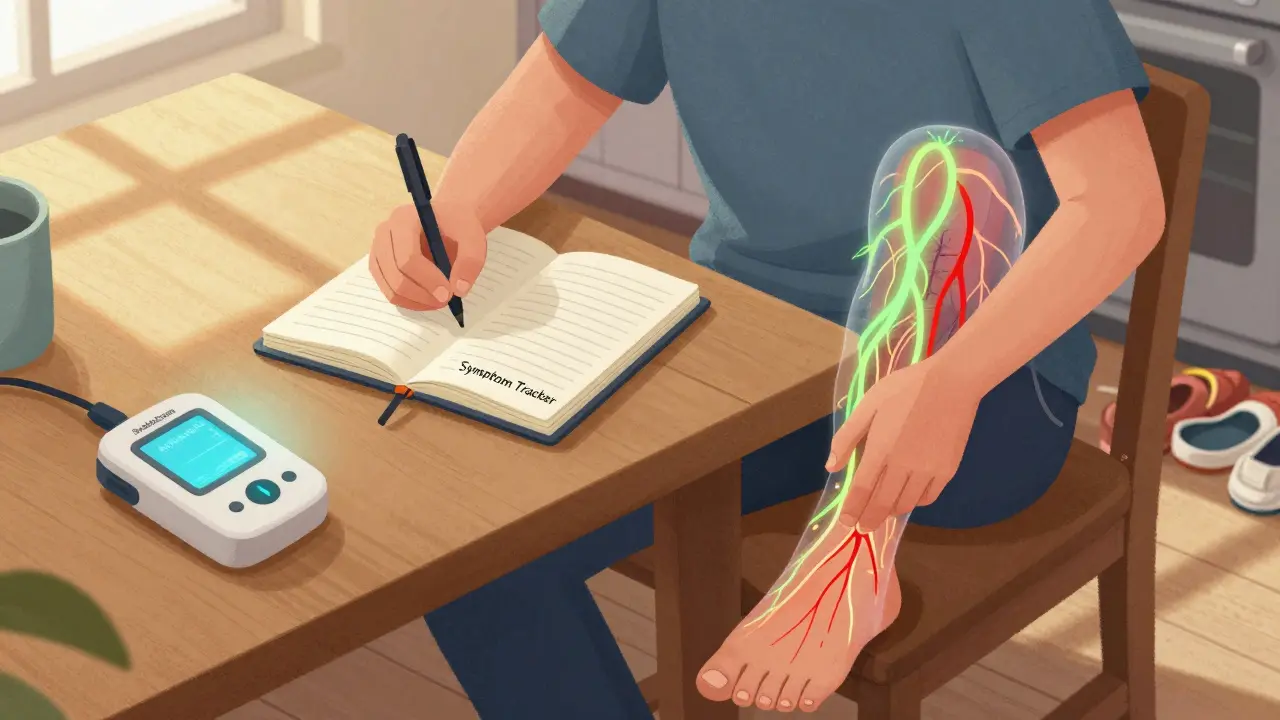
- Track your symptoms. Write down when the tingling started, where it is, and if it’s getting worse. This helps your doctor decide if it’s the drug or something else.
- Ask about vitamin B6. For isoniazid, doctors often prescribe it to prevent neuropathy. It’s not a cure-all, but it helps in some cases.








Diana Alime
24 Dec 2025 at 00:02so i started taking metronidazole for that weird infection and my toes went numb like wtf
doc said "it's normal" so i kept going
now i can't feel my feet when i walk and i tripped over my own dog
why do they act like this is just a side effect like a sneeze??