Medication Safety Checker
Check for dangerous drug interactions and safety reminders. Enter medications your family member takes to identify potential risks and get personalized safety tips.
Why a Shared Medication Calendar Matters
Imagine your parent takes eight different pills a day-some with food, some without, some at 7 a.m., others at 10 p.m. One dose is skipped. Another is doubled. A dangerous interaction happens. This isn’t rare. Nearly 125,000 people in the U.S. die each year because of medication errors, and most of them happen at home. The problem isn’t that people forget. It’s that no one has a clear, shared view of what’s being taken, when, and by whom.
A shared medication calendar isn’t just a digital to-do list. It’s a safety net. It stops missed doses, prevents dangerous drug clashes, and spreads the weight of caregiving across multiple people. In 2020, 53 million Americans were unpaid caregivers. Most of them are exhausted. A good system doesn’t just help the person taking meds-it protects the people trying to help.
What a Shared Medication Calendar Actually Does
At its core, a shared medication calendar tracks three things: what medicine is taken, when it’s taken, and who’s responsible. But the best ones do more. They warn about drug interactions. They send alerts to multiple people at once. They let you assign tasks like picking up prescriptions or checking if someone ate before taking their pill.
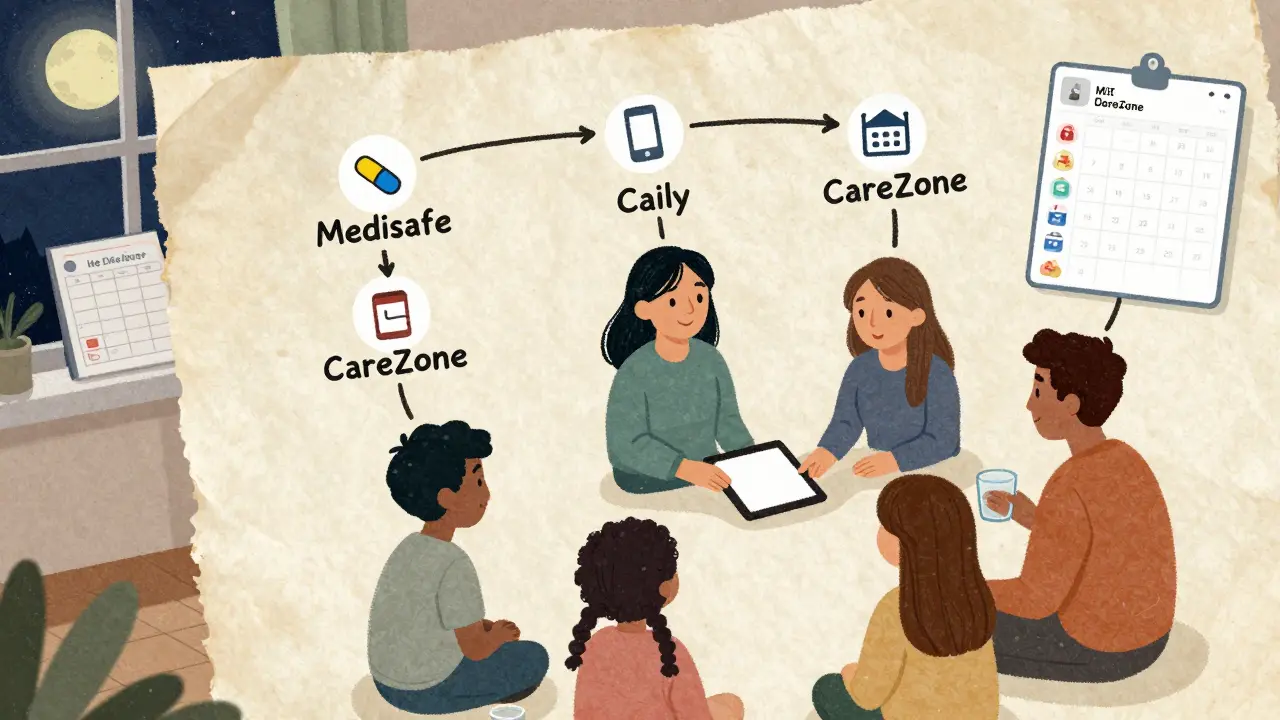
Standard calendar apps like Google Calendar or Apple Calendar can track times. But they don’t know that warfarin can’t be taken with ibuprofen, or that metformin should be taken with food. Specialized apps like Medisafe, Caily, and CareZone were built for this. They have databases of over 650,000 drug combinations. If someone adds a new prescription, the app flags risks before they happen.
And it’s not just about reminders. A 2022 Johns Hopkins study found that families using healthcare-specific apps saw a 47% drop in missed doses compared to those using regular calendars. That’s not a small gain. That’s life or death.
Choosing the Right Tool: Free vs. Specialized Apps
You don’t need to spend money to start. Google Calendar is free, works on any device, and lets you share with anyone with an email. But here’s the catch: you have to type everything in manually. No drug warnings. No pharmacy sync. No task assignments. It’s like using a flashlight to find your way in a storm-better than nothing, but not enough.
Apple Calendar is great if everyone uses iPhones. It syncs with the Health app and works with Siri. But if your sister uses an Android phone? She’s out of the loop. Microsoft Outlook is powerful but clunky for non-tech users. Most caregivers over 50 struggle with it, according to AARP’s 2022 survey.
Specialized apps fix this:
- Medisafe: Best for medication safety. Tracks 650,000+ drug interactions, has 98.7% accuracy in dose tracking, and sends alerts to up to 10 people. Free version limits sharing. Premium is $9.99/month.
- Caily: Best for family coordination. Lets you assign chores like "buy groceries" or "drive to pharmacy" alongside medication times. Free for up to 5 people. Premium is $9.99/month.
- CareZone: Best for pharmacy integration. Imports prescriptions automatically from your pharmacy. Free version works fine. Premium is $5.99/month. Usability scores are lower for seniors, though.
Only 22% of caregivers use apps with these features. The rest rely on sticky notes, phone calls, or memory. That’s risky.

How to Set It Up Right (Step by Step)
Setting up a shared calendar isn’t about tech skills. It’s about teamwork. Here’s how to do it without stress:
- Have the first meeting. Gather everyone involved-spouse, kids, neighbors, visiting nurses. Talk about what meds are taken, when, and why. Write it down together. Don’t assume anyone knows the full list.
- Choose one calendar. Pick one platform and stick with it. Don’t use Google for one person and Apple for another. Sync issues will break trust.
- Create a separate calendar. Don’t mix meds with birthdays and appointments. Name it "Mom’s Meds" or "Dad’s Care Schedule." This keeps things clear and private.
- Add every dose. Include the name, dose, time, and instructions: "Take with food," "Avoid alcohol," "Check BP before taking." Be specific.
- Set reminders 15 minutes early. Most people need time to get water, sit down, or find their pills. A 7 a.m. reminder won’t work if they’re still brushing their teeth.
- Assign roles. Who picks up prescriptions? Who checks if the pillbox is full? Who calls the pharmacy if something’s wrong? Write it down.
- Give everyone access. Don’t lock it behind one person. If the main caregiver gets sick, someone else needs to step in-immediately.
Studies show that families who follow this process reduce coordination errors by 63%. That’s the difference between chaos and calm.
Privacy and Trust: The Hidden Challenge
Not everyone wants their family seeing every health detail. In fact, 68% of older adults worry about privacy when sharing medication info, according to the National Council on Aging. That’s valid. A daughter shouldn’t see her parent’s mental health meds unless she needs to.
Here’s how to handle it:
- Use apps with role-based access. Medisafe lets you choose who sees what. You can hide sensitive meds from some people.
- Don’t share passwords. Use the app’s built-in sharing feature. Never give someone your Google or Apple login.
- Have a conversation about boundaries. "I’m okay with you seeing my blood pressure meds, but not my antidepressants." Say it out loud.
- Use a printed backup. Some seniors don’t trust screens. Keep a paper copy in a drawer. Update it weekly.
Dr. Richard Frankel warns in Health Affairs that digital tools create false security. If someone ignores a notification, the system fails. That’s why human checks matter. A daily phone call from a sibling or a quick visit from a neighbor still beats any app.
What to Do When Things Go Wrong
Technology fails. Phones die. Notifications get silenced. Someone forgets to update the calendar. That’s normal. The goal isn’t perfection. It’s resilience.
Here’s how to recover:
- Notifications ignored? Set up a backup text or call chain. If no one responds to the app alert in 30 minutes, the next person gets a call.
- Sync issues? Use a single device as the source of truth. Update it first, then check others.
- Someone adds the wrong dose? Have a weekly 10-minute check-in. Review the calendar together. Say: "Does this still match what the pharmacist said?"
- App crashes? Print the schedule. Keep it by the pillbox. Use a whiteboard on the fridge.
67% of successful setups include a printed backup, according to the Senior Living Research Group. Don’t skip this. Tech is a tool, not a replacement for human care.
What’s Next: The Future of Medication Safety
Apps are getting smarter. Medisafe now uses AI to predict when someone is likely to miss a dose-based on past behavior. Apple’s iOS 17 can auto-create medication schedules from prescription data. Google’s new Healthcare Mode for Calendar lets you pick from pre-built templates like "Diabetes Meds" or "Heart Failure Regimen." By 2027, 95% of healthcare systems in the U.S. are expected to offer integrated medication calendars. Kaiser Permanente already did-cutting ER visits by 31% in just two years.
But tech alone won’t fix this. The real breakthrough is when families stop seeing medication management as a chore and start seeing it as a shared responsibility. That’s what saves lives.
Start Small. Stay Consistent.
You don’t need to build a perfect system on day one. Start with one person’s three most important pills. Add one family member. Set one reminder. Check it for a week. Then add another. Slow progress beats no progress.
Medication safety isn’t about having the fanciest app. It’s about making sure no one has to take a pill alone. And no one has to carry the weight alone, either.





Josh josh
26 Jan 2026 at 02:53bro i just started using medisafe for my grandma and holy crap it actually works. no more screaming at my sister because she forgot to refill her blood pressure pills. i set up alerts for me and my aunt and now we get pings when she skips a dose. its like having a robot nurse who never sleeps.
also the free version is fine if you dont need 10 people on it. just add the essentials.