For decades, rheumatoid arthritis (RA) meant a slow, painful decline. Joint damage, constant fatigue, and loss of function were seen as inevitable. But that’s no longer the truth. Today, biologic DMARDs have changed everything. They don’t just ease symptoms-they can stop the disease in its tracks. For many people, remission isn’t a dream anymore. It’s a real, achievable outcome.
What Are Biologic DMARDs and How Do They Work?
Biologic DMARDs are targeted drugs designed to block specific parts of the immune system that go haywire in rheumatoid arthritis. Unlike older drugs like methotrexate that broadly suppress immunity, biologics act like precision missiles. They target only the molecules driving inflammation-like TNF-alpha, IL-6, or T-cells-leaving the rest of your immune system mostly intact. These drugs didn’t appear overnight. The first one, etanercept (Enbrel), was approved by the FDA in 1998. Since then, more than a dozen have followed. They’re grouped by what they block:- TNF inhibitors: etanercept, adalimumab, infliximab, golimumab
- IL-6 blockers: tocilizumab
- T-cell modulators: abatacept
- B-cell depleters: rituximab
- IL-1 blockers: anakinra
Who Gets Biologic DMARDs?
Not everyone with RA starts with a biologic. The American College of Rheumatology recommends methotrexate first. It’s cheap, well-studied, and works for many. But if you’re still in pain after 3-6 months on methotrexate-or if your joints are already showing damage on X-rays-it’s time to consider a biologic. About 30% of RA patients eventually need one. That’s not because methotrexate failed them personally-it’s because RA is unpredictable. Some people respond beautifully to it. Others don’t. And for those who don’t, the damage keeps moving forward. Biologics are the next step to stop it.Can Biologics Actually Bring Remission?
Yes. And that’s the biggest shift in RA care in 50 years. In clinical trials, 20-50% of patients on biologics achieve remission. That’s compared to just 5-15% on methotrexate alone. Remission doesn’t mean you’re cured. It means your disease is quiet. No swelling. No morning stiffness. No fatigue dragging you down. Blood tests show normal inflammation levels. X-rays stop showing new damage. Real-world data backs this up. A 2022 study in the Journal of Rheumatology found that patients on biologics were nearly twice as likely to reach low disease activity or remission compared to those on traditional drugs. One patient, diagnosed 15 years ago with severe RA, reported remission within eight weeks of starting tocilizumab. That’s not rare anymore.
Not All Biologics Are the Same
Choosing the right one isn’t guesswork anymore. Studies show clear differences in how well each works. A 2022 review in Exploration Medicine found that adalimumab, etanercept, and golimumab were 19% more effective than infliximab in real-world settings. And non-TNF biologics like tocilizumab and abatacept often outperform TNF blockers in certain patient groups. Why? Because RA isn’t one disease. It’s many. Some people’s RA is driven by too much TNF. Others by IL-6 or B-cells. If your body’s main problem is IL-6, giving you a TNF blocker might not help much. But tocilizumab? That could be a game-changer. Synovial tissue testing is starting to help doctors match patients to the right drug. One study found that only 12% of patients with low B-cell signatures responded to rituximab-but 50% responded to tocilizumab. This isn’t science fiction anymore. It’s becoming standard practice in top rheumatology clinics.Cost and Access: The Big Hurdle
There’s no sugarcoating this: biologics are expensive. In the U.S., annual costs range from $50,000 to $70,000 per person. That’s 5 to 10 times more than methotrexate. But biosimilars are changing the game. Since 2016, copies of originator drugs like adalimumab and etanercept have entered the market. They’re just as effective, but 15-30% cheaper. By Q2 2023, biosimilars made up 35% of TNF inhibitor prescriptions in the U.S. Many patients on biosimilars report 27% lower out-of-pocket costs. Still, getting approved can take weeks. Insurance companies often require step therapy-meaning you must try methotrexate first, then maybe another DMARD, before they’ll cover a biologic. Specialty pharmacies help with paperwork, and manufacturer assistance programs can cover 40-100% of costs for qualifying patients.Side Effects and Risks
Biologics aren’t risk-free. Because they dampen parts of your immune system, you’re more vulnerable to infections. Serious infections-like tuberculosis, pneumonia, or sepsis-can happen. That’s why doctors test for TB before starting treatment. Injection site reactions are common with subcutaneous drugs (like adalimumab or etanercept). About 45% of adverse event reports mention redness, itching, or swelling at the injection spot. Most fade with time. Some patients worry about cancer risk. Studies show a small increase in certain skin cancers, but no clear link to lymphoma or other major cancers in RA patients on biologics. The risk is higher if you’ve had cancer before, so discuss your history with your doctor. One big concern: secondary failure. About 40% of patients who respond well at first start losing effectiveness after 12-24 months. That doesn’t mean the drug stopped working-it means your body adapted. Switching to a different class of biologic often helps. But each new one tends to work less well than the last. That’s why choosing the right one the first time matters.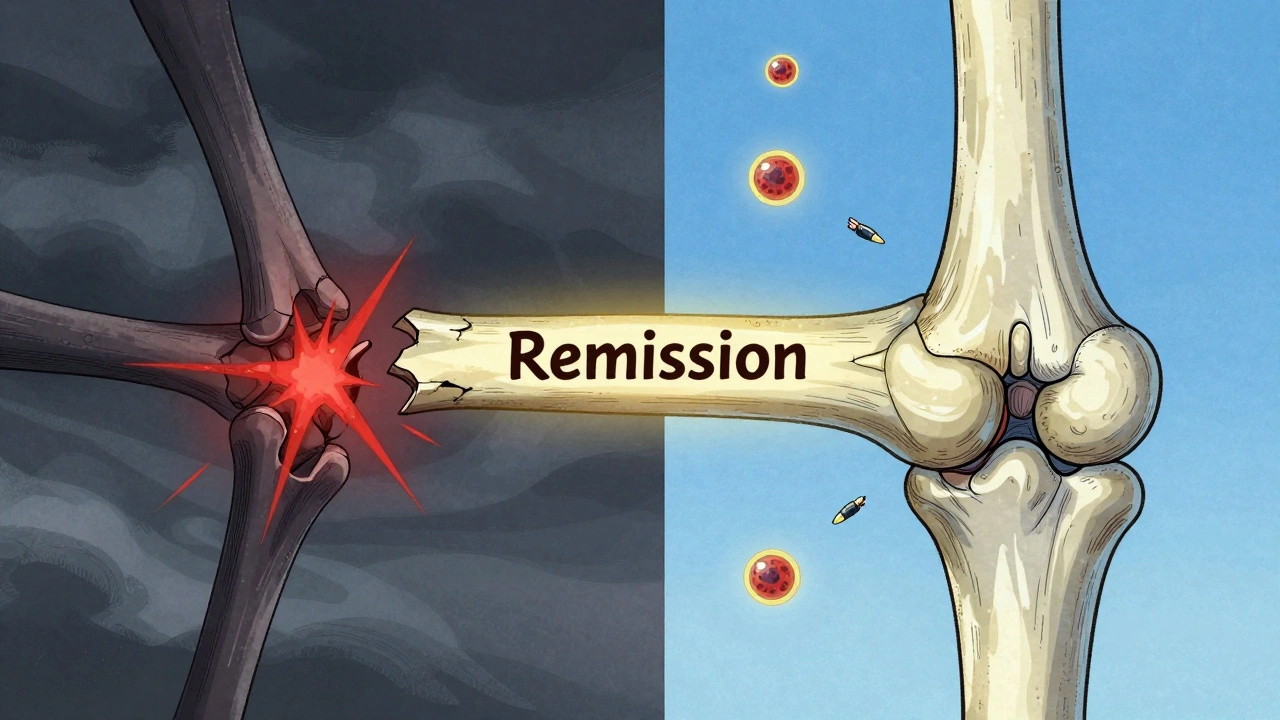
What It’s Like to Use Them
Most biologics are self-injected at home. You’ll get trained by a nurse-usually two sessions are enough. Many patients say it’s easier than they expected. The pens are small, the needles are fine, and the process takes less than a minute. Some, like infliximab, require IV infusions every 4-8 weeks at a clinic. That’s more time-consuming but avoids the anxiety of self-injection. Patients on Drugs.com gave adalimumab a 4.2/5 satisfaction rating across over 2,300 reviews. The most common praise? “I can hold my grandkids again.” “I slept through the night for the first time in years.” “I went back to work.” But the emotional toll is real too. The fear of infection. The stress of insurance battles. The guilt of being “that expensive patient.” Support groups, like the Arthritis Foundation’s forums, help. So do apps like ArthritisPower, which let you track symptoms, meds, and side effects over time.The Future: Personalized Treatment and Beyond
The next wave of RA treatment is personalization. Researchers are looking at genetic markers, blood proteins, and even joint tissue samples to predict which drug will work best for you-before you even start. New drugs are coming too. Upadacitinib (Rinvoq), a JAK inhibitor, showed better results than adalimumab in head-to-head trials. Baricitinib achieved 28% higher remission rates in some studies. Longer-acting versions are in trials-like a tocilizumab injection that works for six months instead of four. By 2027, biosimilars are expected to make up 60% of the biologic market. That means more people will have access. But the big challenge remains: 30-40% of patients still don’t respond to any biologic. Finding better predictors-and better drugs-is the next frontier.What You Can Do Now
If you have RA and aren’t in remission:- Ask your rheumatologist about your disease activity score (DAS28). Are you still in moderate or high disease activity?
- Have you tried methotrexate for at least 3-6 months at a full dose?
- Do you have joint damage visible on X-rays or ultrasound?
Can biologic DMARDs cure rheumatoid arthritis?
No, biologic DMARDs cannot cure rheumatoid arthritis. But they can induce remission-meaning the disease becomes inactive and symptoms disappear. Many patients stay in remission for years with continued treatment. Stopping the medication often leads to flare-ups, so most people need to stay on it long-term.
How long does it take for biologic DMARDs to work?
TNF inhibitors like adalimumab or etanercept often start working in days to weeks. Non-TNF biologics like abatacept or tocilizumab may take 6-12 weeks to show full effect. Most patients see noticeable improvement within 3 months. If there’s no change by then, your doctor may switch you to a different drug.
Are biosimilars as effective as the original biologics?
Yes. Biosimilars are highly similar to the original biologic drugs in structure, function, and effectiveness. The FDA requires them to show no meaningful clinical differences in safety or effectiveness. Many patients switch from originator drugs to biosimilars without losing control of their RA. They’re also significantly cheaper, reducing out-of-pocket costs by 15-30%.
Can I stop taking biologic DMARDs if I feel better?
Most doctors advise against stopping, even if you’re in remission. Stopping treatment increases the chance of a flare-up by 60-80% within a year. Some patients under strict supervision may try tapering slowly, but this should only be done with close monitoring. Never stop on your own.
What are the signs of a serious infection while on biologics?
Watch for fever over 100.4°F (38°C), chills, cough, shortness of breath, red or swollen skin wounds, or unexplained fatigue. These can be signs of serious infections like pneumonia, tuberculosis, or sepsis. If you notice any of these, contact your doctor immediately. Don’t wait. Early treatment saves lives.
Why do some people stop responding to biologics over time?
This is called secondary failure. Your immune system may start producing antibodies against the drug, making it less effective. Or your disease may shift to using different inflammatory pathways. About 40% of patients experience this after 12-24 months. Switching to a biologic with a different mechanism-like moving from a TNF blocker to an IL-6 inhibitor-often restores control.







Maria Elisha
9 Dec 2025 at 17:14Ugh I just got my biologic approved after 3 months of insurance hell. Now I have to learn to inject myself? Like I don’t have enough to deal with already. Can’t they just give us a pill like normal people?