Clozapine ANC Monitoring Schedule Calculator
Calculate your personalized ANC monitoring schedule based on current guidelines. Note: All recommendations are based on clinical practice, not regulatory requirements.
Clozapine’s Safety Rules Changed in 2025 - Here’s What You Need to Know
If you or someone you know takes clozapine for treatment-resistant schizophrenia, the rules around blood tests and pharmacy access just got simpler. As of February 24, 2025, the FDA officially removed the mandatory REMS program for clozapine. That means no more paperwork, no more certified prescribers, and no more pharmacy delays tied to reporting absolute neutrophil count (ANC) results before each refill.
This isn’t a relaxation of safety - it’s a recognition that the system meant to protect patients had become a barrier to care. For years, clozapine, the most effective antipsychotic for people who haven’t responded to other treatments, was underused because of red tape. Now, the focus shifts from government-enforced monitoring to clinical judgment.
What Was the Clozapine REMS Program?
The Risk Evaluation and Mitigation Strategy (REMS) for clozapine started in 2015 as a response to the risk of severe neutropenia - a drop in white blood cells that can lead to life-threatening infections. The FDA first approved clozapine in 1989, but its use was tightly controlled because of this risk. By 2015, the REMS program required every prescriber, pharmacy, and patient to register and follow strict rules.
Here’s how it worked:
- Prescribers had to complete special training and get certified through the Clozapine REMS website.
- Pharmacies had to be certified too - and couldn’t fill prescriptions without proof of recent ANC blood work.
- Patients had to get monthly blood tests and have results submitted to a national registry.
- Each month, clinics had to complete a Patient Status Form and submit it to the REMS system.
- After November 2021, pharmacies could no longer use phone or fax to verify safety - they had to log into the REMS portal.
These steps were meant to prevent fatal cases of agranulocytosis. But in practice, they created delays. A 2022 survey found clinics spent an average of 3.2 hours per week just managing REMS paperwork. For patients in rural areas or those without strong support systems, getting clozapine could take weeks.
Why Did the FDA Remove the Mandatory REMS?
The FDA didn’t ignore the risk. They studied it - hard.
In 2024, they launched a full review using data from the FDA Adverse Event Reporting System, the Sentinel System, and partnerships with the Department of Veterans Affairs and Brigham and Women’s Hospital. They looked at real-world use over the past decade. What they found surprised even some experts:
- Doctors and nurses were already monitoring ANC levels closely - even without the REMS system.
- The risk of severe neutropenia is highest in the first 18 weeks, then drops significantly. But it never disappears.
- Healthcare providers had learned to manage the risk over time. Training, guidelines, and experience replaced the need for a rigid registry.
- Only 0.8% of patients on clozapine developed severe neutropenia, and most cases were caught early thanks to routine monitoring.
The FDA concluded: the REMS program was no longer needed to keep patients safe. The system was working - but it was holding people back.
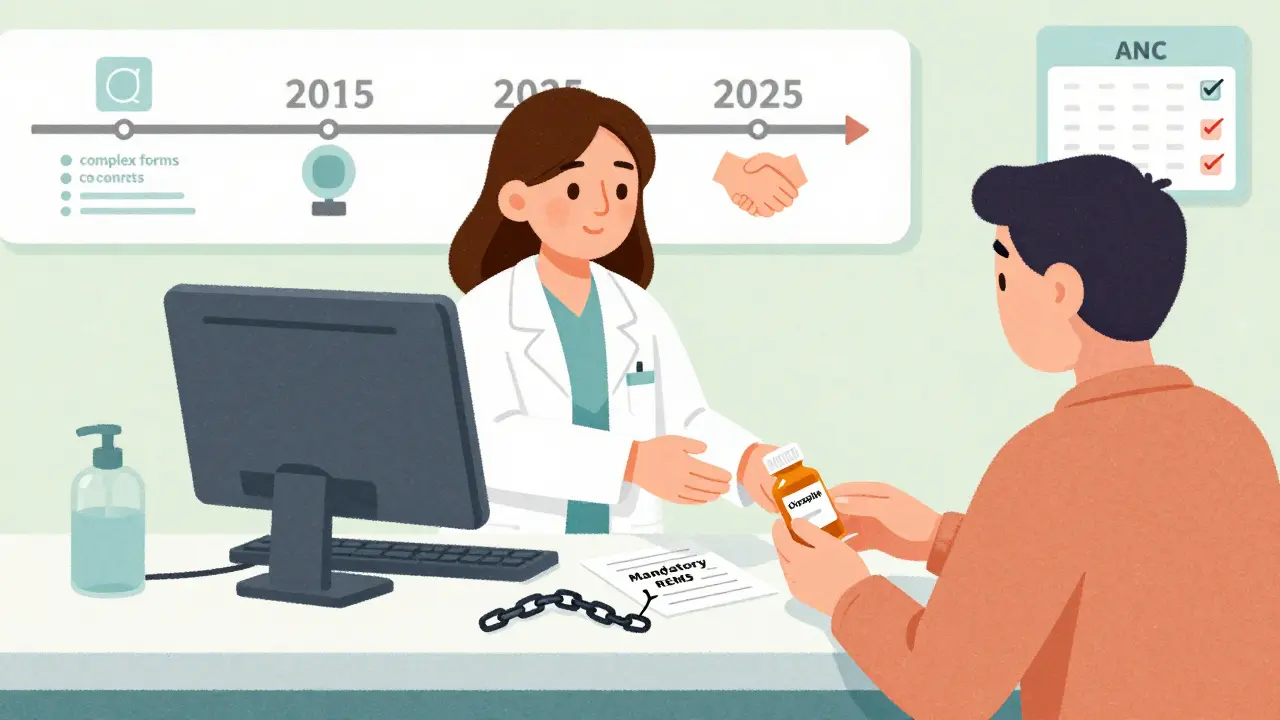
What Changes for Patients and Providers Now?
As of February 24, 2025, the mandatory REMS is gone. That means:
- You no longer need to be enrolled in the Clozapine REMS program.
- Prescribers don’t need to be certified to write clozapine prescriptions.
- Pharmacies can dispense clozapine without checking a central database.
- There’s no more monthly Patient Status Form to fill out.
But here’s what hasn’t changed:
- The boxed warning about severe neutropenia is still on every clozapine label.
- The prescribing information from Novartis still recommends regular ANC monitoring.
- Doctors are still expected to follow the same monitoring schedule:
- Baseline ANC before starting clozapine.
- Weekly tests for the first 6 months.
- Every two weeks from months 6 to 12.
- Monthly after 12 months - with shared decision-making.
For patients with Benign Ethnic Neutropenia (a common, harmless condition in people of African, Middle Eastern, or Mediterranean descent), the threshold is lower: ANC ≥1000/μL instead of ≥1500/μL.
These guidelines aren’t enforced by law anymore - they’re based on medical best practices. That means the responsibility is back where it belongs: between you and your doctor.
Why This Matters for Access to Care
Before the REMS removal, only about 12% of people with treatment-resistant schizophrenia in the U.S. got clozapine - even though it works for 30-50% of those who fail other drugs. That’s not because doctors didn’t want to prescribe it. It was because the system made it too hard.
Patients waited. Clinics turned away cases. Rural pharmacies refused to stock it. A 2023 study found clinics without a dedicated REMS coordinator were nearly four times less likely to start someone on clozapine.
Now, the barriers are gone. Anthem’s Provider News predicts a 25-30% increase in new clozapine starts over the next two years. Evaluate Pharma raised its market forecast from $487 million in 2024 to $612 million by 2026 - not because the drug got more expensive, but because more people can actually get it.
What About Safety? Is This Risky?
Some clinicians worry that without mandatory reporting, someone might miss a blood test. That’s a fair concern.
But the FDA’s research showed something important: providers didn’t stop monitoring when the REMS system was in place. They just did it because it was the right thing to do. The American Psychiatric Nurses Association called the removal “a success for both providers and patients.”
Still, the risk hasn’t vanished. Severe neutropenia can happen at any time - especially in the first few months. That’s why:
- Patients should never skip blood tests without talking to their doctor.
- Doctors should still order ANC tests on schedule - even if no one’s checking.
- Pharmacists should still ask if the patient’s been tested, even if they don’t need proof.
It’s now a matter of professional responsibility, not legal compliance.
What’s Next for Clozapine?
The FDA is not walking away from clozapine safety. They’re just changing how they monitor it.
Manufacturers are updating drug labels to remove REMS references. The American Society of Health-System Pharmacists is rolling out new clinical guidelines in Q3 2025 to help providers stay on track.
The FDA will keep watching through the Sentinel System - their real-time drug safety network. Early data shows monitoring rates haven’t dropped since the REMS ended. That’s a good sign.
For patients, this means faster access. For providers, less paperwork. For everyone, the same goal: getting the right treatment to the right person, without unnecessary roadblocks.
Frequently Asked Questions
Do I still need to get blood tests for clozapine?
Yes. Even though the FDA no longer requires reporting your ANC results, your doctor should still order regular blood tests. The risk of severe neutropenia is highest in the first 6 months and continues at a lower level after that. Skipping tests increases your risk of missing a dangerous drop in white blood cells.
Can any pharmacy fill my clozapine prescription now?
Yes. Pharmacies no longer need to be certified or check a federal database before dispensing clozapine. They can fill your prescription like any other medication. But good pharmacists will still ask if you’ve had your ANC test done - because it’s part of standard care.
Do I need to re-enroll in the REMS program?
No. The mandatory REMS program was removed on February 24, 2025. You are no longer required to enroll, re-enroll, or submit any forms to the Clozapine REMS registry. Your doctor and pharmacy won’t ask you for REMS paperwork anymore.
Is clozapine still considered dangerous?
It carries a serious risk - severe neutropenia - which is why the boxed warning remains on the label. But the risk is well understood and manageable with regular blood tests. Over 30 years of use have shown that with proper monitoring, clozapine is safe for most people. The removal of REMS doesn’t mean the risk is gone - it means we trust doctors to manage it responsibly.
What if my doctor stops ordering blood tests?
If your doctor stops ordering ANC tests, ask why. The prescribing guidelines still recommend monthly testing after 12 months, and weekly testing in the first 6 months. If they say they no longer need to monitor because of the REMS removal, that’s incorrect. The FDA removed the registry - not the medical need for monitoring. You have the right to ask for the tests that keep you safe.








Anthony Massirman
3 Feb 2026 at 10:44Finally. Took them long enough. I've seen patients drop meds because of this bureaucracy. No more excuses now.