Medication Safety Risk Checker
Calculate your personalized risk of medication side effects based on medical history. This tool estimates risk factors but is not medical advice. Always consult your doctor for treatment decisions.
Assess Your Risk Factors
Your Medication Risk Assessment
Recommended Actions
Every time you take a new pill, your body doesn’t start from scratch. It remembers. Your past illnesses, your other medications, your age, your genetics - they all shape how your body reacts to drugs today. That’s why your medical history isn’t just background information. It’s a live risk calculator for side effects.
Why Your Past Illnesses Change How Drugs Work
If you have kidney disease, your body can’t flush out drugs the same way a healthy person can. That means medications like ibuprofen, certain antibiotics, or even diabetes drugs can build up to dangerous levels. The Merck Manual confirms that people with chronic kidney disease clear 50-75% less of many drugs from their system. For some, that turns a normal dose into an overdose. The American Medical Association says 40% of commonly prescribed drugs need dose changes in these patients - but only 35% of electronic systems even flag this risk when doctors write prescriptions.
Same goes for liver problems. Your liver breaks down most medications. If it’s damaged by hepatitis, alcohol, or fatty liver disease, drugs like statins, antidepressants, or painkillers can stay in your blood too long. Genetic differences in liver enzymes - like CYP450 variants - can make drug levels spike by 30% to 500%. That’s not rare. It’s common. And most doctors don’t test for it.
Polypharmacy: The Silent Killer in Your Medicine Cabinet
Taking five or more medications at once? You’re doubling your risk of a bad reaction. Taking ten or more? Your risk triples. That’s not a guess. It’s from the British Heart Foundation’s 2023 analysis of over 200,000 patients. Each extra pill adds 7-10% more risk. Why? Because drugs fight each other. One slows down how your body processes another. Another makes your stomach more sensitive. A third lowers your blood pressure so much that you faint.
It gets worse. A 2020 study in Pakistan found patients on five or more drugs had 1.74 times higher odds of medication errors. And those with multiple chronic conditions - like diabetes, heart disease, and arthritis - had 2.6 times the risk. The Charlson Comorbidity Index, a tool doctors use to predict outcomes, shows every extra condition bumps up your chance of harm. But here’s the problem: most patients don’t know what they’re taking, and many doctors don’t ask.
Age Isn’t Just a Number - It’s a Drug Risk Factor
If you’re over 65, you’re 3 to 5 times more likely to have a bad reaction to a drug than someone under 40. Why? Your body changes. Your kidneys slow down. Your liver works less efficiently. Your body fat increases, and water decreases - which changes how drugs dissolve and spread. The American Geriatrics Society calls this the perfect storm for side effects.
And it’s not just biology. Older adults are more likely to see multiple doctors, fill prescriptions at different pharmacies, and forget doses. That’s how dangerous combinations slip through. Warfarin and NSAIDs - a common mix for arthritis and heart patients - cause over 34,000 emergency room visits in the U.S. every year, according to CDC data. Many of those cases could’ve been avoided if someone had looked at the full history.
Gender Matters More Than You Think
Women over 65 experience adverse drug reactions at least 50% more often than men. That’s not because they’re more sensitive. It’s because most drug trials were done on men. Between 2010 and 2020, only 22% of participants in cardiovascular drug studies were women. So dosing guidelines were built on male biology. But women metabolize drugs differently. They have less body water, more body fat, and different liver enzyme activity. A drug that’s safe for a man might be toxic for a woman - especially after menopause.
And it’s not just hormones. Women are more likely to take multiple medications for chronic conditions - and more likely to be prescribed drugs with known gender-specific risks, like certain antidepressants or blood pressure pills. Yet, few doctors adjust doses based on sex. That’s a gap in care - and a hidden danger.
History of Allergies and Cross-Reactions
If you had a bad reaction to penicillin, you’re not just allergic to penicillin. You’re at eight times higher risk of reacting to cephalosporins - a different class of antibiotics. Why? They look similar to your immune system. That’s called cross-reactivity. A 2009 study found patients with one drug allergy had a 30-40% higher chance of reacting to another drug in the same family.
And it’s not just allergies. If you’ve ever had muscle pain from a statin, you’re more likely to get it again - even with a different statin. If you got dizzy from a blood pressure pill, you might react badly to others in the same group. Your body learns. And if your doctor doesn’t know your history, they might repeat the same mistake.

What You Don’t Tell Your Doctor Can Hurt You
Patients often leave out key details. They forget about herbal supplements. They don’t mention they stopped a pill because it made them sick. They skip doses to save money - then restart without telling anyone. That’s dangerous. The American Medical Association found 25% of patients skip meds due to cost. When they restart, their body isn’t ready. That leads to 28% more side effects.
And here’s the scary part: 62% of people with three or more chronic conditions say their doctors didn’t realize their symptoms were caused by a drug. They thought it was their heart failing, their arthritis flaring, or their dementia getting worse. But it was a side effect - one that could’ve been fixed by adjusting the dose or switching meds. The Merck Manual says: always consider drugs as a cause of new symptoms. But few do.
What You Can Do Right Now
You don’t need a PhD to protect yourself. Here’s what works:
- Keep a real-time list of every pill, vitamin, and supplement you take - including doses and why you take them. Update it every time something changes.
- Bring it to every appointment - even if you think it’s not important. That herbal tea? That OTC painkiller? It matters.
- Ask: “Could this be a side effect?” If you feel new fatigue, dizziness, confusion, or nausea, say it out loud. Don’t assume it’s your condition.
- Request a medication review if you take five or more drugs. The Cochrane Review shows structured reviews reduce side effects by 22%. Yet only 18% of eligible patients get one.
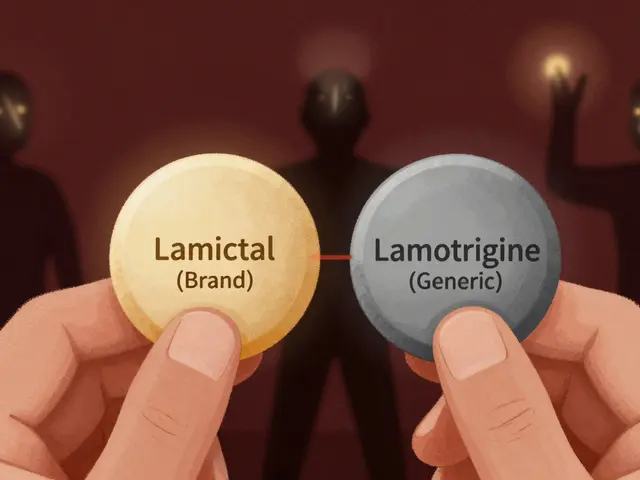
- Ask about pharmacogenomics - especially if you’ve had bad reactions before. New tests can check your genes for how you process drugs. The FDA cleared YouScript in 2023. It’s not everywhere yet - only 5.7% of U.S. clinics use it - but it’s growing.
The Bottom Line
Your medical history isn’t just a file in a cabinet. It’s a map of your body’s hidden vulnerabilities. Every past illness, every drug you’ve taken, every change in your health - it all adds up. And if your doctor doesn’t see the full picture, you’re at risk.
The system isn’t perfect. Electronic records miss key details. Doctors are rushed. Patients forget. But you can change that. You’re the only one who knows your full story. Don’t let it stay hidden. Bring it out. Ask the questions. Push for a review. Your next pill could be safe - or it could be dangerous. The difference? Your history - and whether you share it.
Can my past drug reactions predict future side effects?
Yes. If you’ve had a bad reaction to one drug, you’re more likely to react to others in the same class. For example, a penicillin allergy increases your risk of reacting to cephalosporins by up to eight times. Cross-reactivity happens because similar chemical structures confuse your immune system or liver enzymes. Always tell your doctor about past reactions - even if they happened years ago.
Why do older adults have more medication side effects?
As you age, your kidneys and liver process drugs more slowly. Your body composition changes - more fat, less water - which affects how drugs spread and stay in your system. You’re also more likely to take multiple medications, increasing the chance of dangerous interactions. Studies show people over 65 experience 3-5 times more adverse reactions than younger adults. This isn’t just aging - it’s a pharmacological vulnerability that needs active management.
Does gender affect how drugs work in my body?
Absolutely. Women metabolize many drugs differently than men due to differences in body fat, liver enzymes, and hormone levels. For decades, clinical trials mostly used male subjects, so dosing guidelines were based on male physiology. This means women often get doses that are too high for their bodies - leading to more side effects. Older women, in particular, have at least 50% higher rates of adverse reactions than men, especially with heart and psychiatric medications.
What is polypharmacy, and why is it risky?
Polypharmacy means taking five or more medications at the same time. It’s common in older adults and those with chronic conditions. But each extra drug increases your risk of side effects by 7-10%. That’s because drugs interact - one can slow how another is broken down, or increase its concentration in your blood. People on 10+ drugs have over three times the risk of a serious reaction. The British Heart Foundation calls this one of the biggest preventable causes of hospital admissions.
Can I reduce my risk of medication side effects?
Yes. Keep an up-to-date list of all your medications. Ask your doctor or pharmacist for a medication review - especially if you take five or more drugs. Ask if any side effects you’re feeling could be drug-related. Request genetic testing if you’ve had repeated bad reactions. And never stop or restart a drug without talking to your provider. Structured reviews and deprescribing can reduce side effects by 22%.
Why do doctors sometimes miss drug side effects?
Many doctors don’t have full access to a patient’s complete history - especially if prescriptions come from different clinics or pharmacies. Electronic records often don’t flag key risks like kidney disease or past allergies. Also, side effects can mimic disease symptoms - like beta-blockers hiding fast heartbeat in bleeding, or steroids masking pain from a perforated ulcer. The Merck Manual says drugs should always be on the differential diagnosis list. But most don’t check.
Is genetic testing for drug reactions worth it?
If you’ve had multiple bad reactions to medications, yes. Tests like YouScript analyze 27 gene-drug interactions to predict how your body processes common drugs. Studies show they can reduce side effects by 34% in people with relevant genetic variants. But adoption is low - only 5.7% of U.S. clinics use them as of 2024. Still, if you’re on several meds or have a family history of bad reactions, it’s worth asking your doctor about.




Cara Hritz
21 Dec 2025 at 21:36okay but like i just took a blood thinner and my doc didnt even ask about that herbal tea i drink every morning 😭 i thought it was just 'natural' so it was fine?? turns out it was messing with my INR levels?? like why is this not standard??