Antidepressant Decision Tool
Find the best antidepressant for your needs
This tool helps you understand which antidepressant might work best based on your symptoms and concerns. It's not a replacement for medical advice, but can help you discuss options with your doctor.
Primary symptoms
Secondary symptoms
Side effect concerns
Treatment history
Your Recommendation
Why this might work for you:
Asendin, the brand name for amoxapine, is a tricyclic antidepressant (TCA) that’s been around since the 1980s. It’s not prescribed as often today as it once was, but it still shows up in treatment plans-especially when other antidepressants haven’t worked. If you’re considering Asendin or have been prescribed it, you’re probably wondering: are there better or safer options? This guide breaks down how amoxapine stacks up against today’s most common antidepressants, what real patients experience, and when switching might make sense.
What is Amoxapine (Asendin) and How Does It Work?
Amoxapine is a tricyclic antidepressant that works by increasing levels of serotonin and norepinephrine in the brain. Unlike newer antidepressants like SSRIs, it also has a mild dopamine-blocking effect, which is why some doctors use it for depression with anxiety or agitation. It’s not a first-line treatment anymore, but it’s still effective for treatment-resistant depression. A 2022 review in the Journal of Clinical Psychiatry found that TCAs like amoxapine had similar response rates to SSRIs in patients who hadn’t improved with other meds.
But there’s a catch. Amoxapine comes with more side effects than newer drugs. Common ones include dry mouth, drowsiness, constipation, blurred vision, and weight gain. More serious risks include heart rhythm changes, low blood pressure when standing up, and seizures at higher doses. It’s also toxic in overdose-far more than SSRIs. That’s why many doctors avoid prescribing it unless absolutely necessary.
SSRIs: The Most Common Alternatives
Selective serotonin reuptake inhibitors (SSRIs) like sertraline (Zoloft), escitalopram (Lexapro), and fluoxetine (Prozac) are now the go-to for depression. They’re easier to tolerate, safer in overdose, and have fewer drug interactions. A 2023 meta-analysis of over 500,000 patients showed SSRIs had a 55% response rate compared to amoxapine’s 58%-but with 40% fewer dropouts due to side effects.
Here’s how they compare:
| Feature | Amoxapine (Asendin) | Sertraline (Zoloft) | Escitalopram (Lexapro) | Fluoxetine (Prozac) |
|---|---|---|---|---|
| Class | Tricyclic antidepressant | SSRI | SSRI | SSRI |
| Typical starting dose | 25-50 mg/day | 25-50 mg/day | 10 mg/day | 20 mg/day |
| Time to effect | 2-6 weeks | 2-6 weeks | 2-6 weeks | 2-8 weeks |
| Common side effects | Drowsiness, dry mouth, constipation, dizziness, weight gain | Nausea, insomnia, sexual dysfunction | Nausea, fatigue, sexual dysfunction | Nausea, insomnia, jitteriness |
| Overdose risk | High-can cause seizures, heart arrhythmias | Low-usually non-fatal | Low | Low |
| Drug interactions | Many-especially with other CNS depressants | Moderate-mainly with blood thinners | Moderate | Moderate |
| Used for anxiety? | Yes, especially with agitation | Yes-first choice for OCD and panic | Yes-first choice for generalized anxiety | Yes-long half-life helps with withdrawal |
Most patients prefer SSRIs because they’re easier to live with. You won’t feel as foggy or constipated. Sexual side effects are common with SSRIs, but they’re often reversible after stopping. With amoxapine, the drowsiness and dry mouth can be persistent and harder to manage.
SNRIs: A Middle Ground
Serotonin-norepinephrine reuptake inhibitors (SNRIs) like venlafaxine (Effexor) and duloxetine (Cymbalta) are another alternative. They work on both serotonin and norepinephrine-just like amoxapine-but without the anticholinergic side effects. That means less dry mouth, less dizziness, and less risk of heart issues.
Studies show SNRIs work just as well as TCAs for severe depression. In fact, a 2021 trial comparing venlafaxine to amoxapine found no difference in symptom reduction after 8 weeks. But patients on venlafaxine reported fewer side effects and were 3 times more likely to stick with treatment.
SNRIs do have their own issues. They can raise blood pressure, especially at higher doses. And stopping them suddenly can cause brain zaps and flu-like symptoms. But compared to amoxapine, they’re a safer, more predictable option.
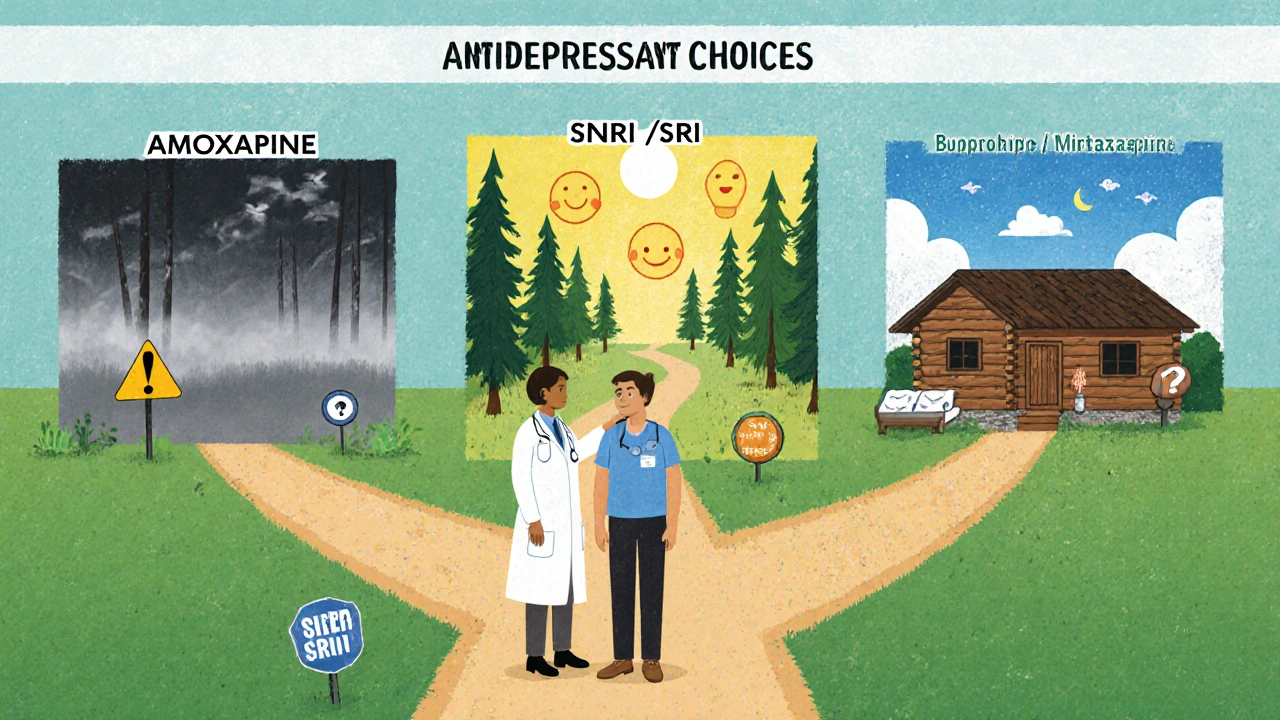
Atypical Antidepressants: Different Mechanisms, Fewer Side Effects
Drugs like bupropion (Wellbutrin), mirtazapine (Remeron), and vortioxetine (Trintellix) work differently than both TCAs and SSRIs. They’re often used when patients can’t tolerate the side effects of other drugs.
Bupropion is popular because it doesn’t cause weight gain or sexual dysfunction. It’s also used for smoking cessation and ADHD. But it can increase anxiety or cause insomnia in some people. It’s not great for depression with high anxiety or agitation-which is where amoxapine sometimes shines.
Mirtazapine is a good fit for people who struggle with sleep and appetite loss. It’s sedating at low doses, which helps with insomnia, and it boosts appetite. But it can cause weight gain and drowsiness. It’s not a direct replacement for amoxapine, but it’s a useful option for patients with those specific symptoms.
Vortioxetine is newer and targets multiple serotonin receptors. It’s been shown to improve not just mood but also thinking and memory in depressed patients. That’s helpful if you’re dealing with brain fog or trouble concentrating. But it’s expensive and not always covered by insurance.
When Might Amoxapine Still Be the Best Choice?
Even with all the newer options, amoxapine isn’t obsolete. It still has a role in specific cases:
- Depression with severe agitation or irritability-amoxapine’s dopamine-blocking effect can calm the nervous system better than SSRIs.
- Patients who’ve tried at least three other antidepressants without success.
- Those with chronic pain and depression-TCAs like amoxapine have pain-relieving properties that SSRIs don’t.
- People who can’t afford newer drugs and need a low-cost option (amoxapine is often under $10 a month in the U.S.)
But even then, doctors usually start low (25 mg) and go slow. They monitor heart rate and ECGs, especially in older adults or those with heart conditions. If you’re on amoxapine, make sure your doctor checks your blood pressure and heart rhythm at least once every 3 months.

What About Natural or Non-Drug Options?
Some people try supplements like St. John’s Wort, omega-3s, or SAM-e as alternatives. But here’s the reality: none of these have been proven as effective as prescription antidepressants for moderate to severe depression. St. John’s Wort can interfere with other medications-including amoxapine-and cause dangerous interactions. The FDA doesn’t regulate supplements like it does drugs, so quality and potency vary wildly.
Therapy, especially cognitive behavioral therapy (CBT), is one of the most effective non-drug treatments. Studies show CBT works as well as antidepressants for mild to moderate depression-and the effects last longer after stopping. Exercise, sleep hygiene, and sunlight exposure also help. But if your depression is severe, these should be used alongside medication, not instead of it.
How to Decide What’s Right for You
There’s no one-size-fits-all antidepressant. The best choice depends on your symptoms, medical history, and lifestyle.
Ask yourself:
- Do I have trouble sleeping or eating? → Mirtazapine might help.
- Am I anxious or agitated? → Amoxapine or an SNRI could be better than an SSRI.
- Do I hate weight gain or sexual side effects? → Bupropion is the best bet.
- Am I on other medications? → SSRIs and SNRIs have fewer interactions than amoxapine.
- Do I need something cheap? → Amoxapine is one of the cheapest options.
And remember: switching antidepressants isn’t instant. It takes 4-6 weeks to know if a new drug is working. Never stop amoxapine suddenly-withdrawal can cause nausea, dizziness, and even seizures. Always taper under a doctor’s supervision.
Final Thoughts: Is Amoxapine Worth It?
Amoxapine works-but it’s not the easiest drug to live with. For most people, SSRIs or SNRIs are safer, better tolerated, and just as effective. If you’re on amoxapine and doing well with no side effects, there’s no reason to switch. But if you’re struggling with drowsiness, dry mouth, or dizziness, or if you’re worried about long-term heart risks, talk to your doctor about alternatives.
The goal isn’t to find the strongest drug-it’s to find the one that lets you feel better without making your life harder.
Is amoxapine still prescribed today?
Yes, but rarely as a first choice. It’s mostly used for treatment-resistant depression or when patients have agitation or chronic pain. Most doctors prefer SSRIs or SNRIs because they’re safer and easier to tolerate.
Can I switch from amoxapine to an SSRI safely?
Yes, but it must be done carefully. Because amoxapine stays in your system longer than SSRIs, your doctor will likely taper you off slowly over 2-4 weeks before starting the new medication. Jumping straight from one to the other can cause serotonin syndrome or withdrawal symptoms.
Does amoxapine cause weight gain?
Yes, weight gain is common with amoxapine, especially over time. It’s more likely than with SSRIs like sertraline or fluoxetine, but less than with mirtazapine. If weight gain is a concern, bupropion or vortioxetine are better options.
Is amoxapine better than Lexapro for anxiety?
For generalized anxiety or panic disorder, Lexapro (escitalopram) is usually preferred. It’s proven effective, safer, and has fewer side effects. Amoxapine might help if your anxiety is tied to severe agitation or irritability, but it’s not the first choice.
How long does it take for amoxapine to work?
Most people start noticing improvements in mood and energy after 2-3 weeks, but full benefits usually take 6-8 weeks. Don’t give up too soon-but if you’re having serious side effects after 2 weeks, talk to your doctor.
Can amoxapine be used for chronic pain?
Yes. Like other tricyclic antidepressants, amoxapine can help with nerve pain, fibromyalgia, and other chronic pain conditions. It’s often used at lower doses (10-50 mg) for pain than for depression. But it’s not FDA-approved for this use, so it’s considered off-label.








Dana Dolan
19 Nov 2025 at 20:06Been on amoxapine for 8 months now-honestly? It saved my life when SSRIs left me numb as a brick. The drowsiness? Yeah, I nap after dinner. The dry mouth? Chews gum like a maniac. But the fog lifted, and I finally slept through the night. No regrets. Just wish docs talked more about TCAs instead of acting like they’re medieval torture devices.