TL;DR
- Both alcohol and tobacco blunt innate and adaptive immunity.
- Alcohol disrupts gut barrier, lowers white‑blood‑cell activity, and skews cytokine production.
- Tobacco introduces oxidative stress, impairs macrophages and neutrophils, and reduces vaccine effectiveness.
- Combined use multiplies infection risk and slows recovery.
- Quitting, balanced nutrition, and regular exercise restore immune resilience faster than you think.
Ever wonder why a night of heavy drinking or a pack of cigarettes seems to leave you feeling “run down”? The answer lies in how these substances hijack the alcohol immune system relationship. Below we break down the biology, compare the two culprits, and give you practical steps to keep your defenses running at full speed.
What the Immune System Actually Does
Immune system is a network of cells, tissues, and organs that identifies and eliminates pathogens, damaged cells, and foreign substances. It works on two fronts:
- Innate immunity - the first line of defense (skin, mucous membranes, phagocytes like macrophages and neutrophils).
- Adaptive immunity - a tailored response driven by lymphocytes including B‑cells that make antibodies and T‑cells that kill infected cells..
Key messengers called cytokines are proteins that coordinate inflammation, cell recruitment, and healing. When everything works as designed, you fend off colds, recover from wounds quickly, and even respond well to vaccines.
Alcohol’s Direct Assault on Immunity
Alcohol is a small, water‑soluble molecule that can cross cell membranes and affect many organ systems. Its impact on the immune system is dose‑dependent but even moderate intake leaves a trace.
1. Disrupting the Gut‑Barrier Shield
The gut houses ~70% of the body’s immune cells. Alcohol increases intestinal permeability, letting bacterial fragments (LPS) leak into circulation. This triggers chronic low‑grade inflammation and forces the liver’s Kupffer cells into overdrive, draining resources from other immune tasks.
2. Weakening Innate Fighters
Studies on chronic drinkers show a 30% reduction in white blood cells especially neutrophils and monocytes, which are crucial for early pathogen clearance.. Their chemotactic ability - the knack to chase microbes - drops by roughly a third, meaning infections set in slower but spread faster.
3. Skewing Cytokine Balance
Alcohol pushes the cytokine profile toward anti‑inflammatory IL‑10 while suppressing pro‑inflammatory IL‑6 and TNF‑α. The result is a muted fever response and a delayed alert to invading germs.
4. Blunting Adaptive Responses
B‑cell antibody production falls 20% after a binge‑drinking episode, and CD8+ T‑cell cytotoxicity drops by about 15%. This explains why heavy drinkers have poorer outcomes after flu shots.
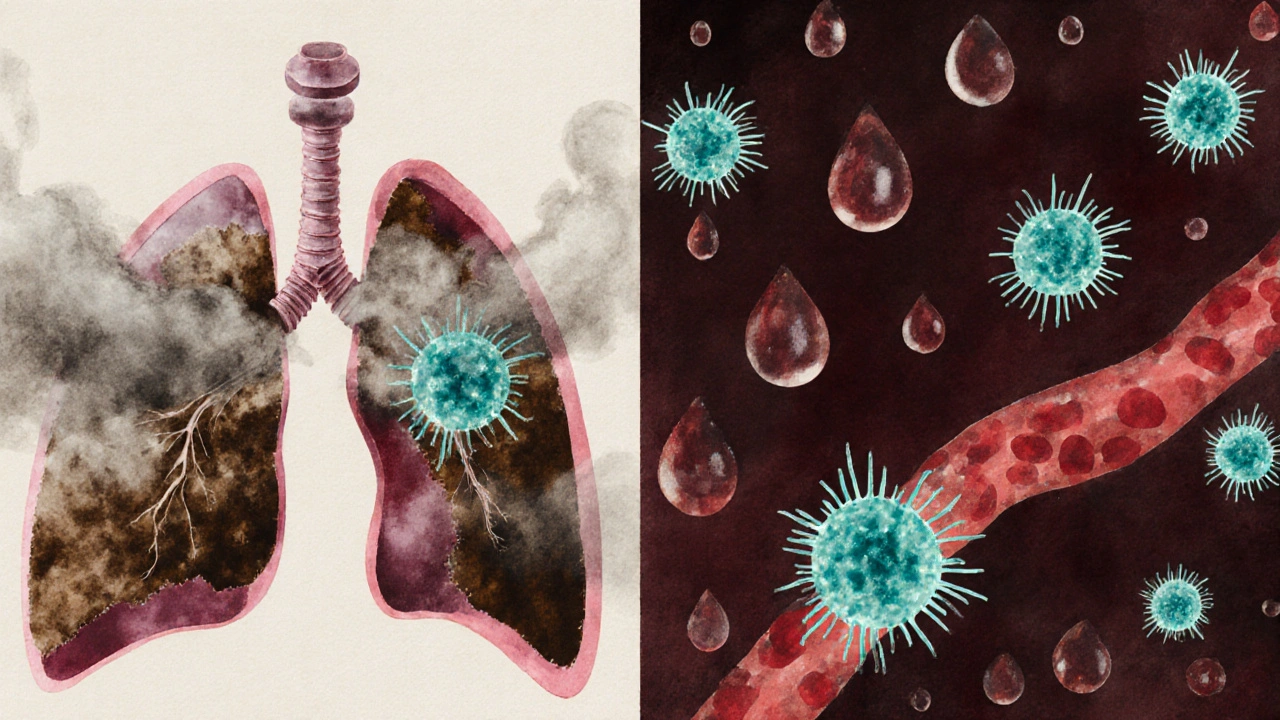
Tobacco’s Multi‑Faceted Attack
Tobacco contains nicotine, tar, and thousands of chemicals that irritate respiratory tissue and enter the bloodstream. Its effect on immunity is both local (lungs) and systemic.
1. Oxidative Stress Overload
Every cigarette puff loads the body with free radicals. Oxidative stress damages cell membranes, DNA, and signaling proteins. Immune cells spend energy repairing this damage instead of fighting microbes.
2. Impaired Macrophage & Neutrophil Function
Alveolar macrophages-those stationed in the lungs-lose up to 40% of their phagocytic ability in smokers. Neutrophil extracellular trap (NET) formation is also reduced, compromising the ability to trap bacteria.
3. Cytokine Imbalance & Chronic Inflammation
Unlike alcohol’s anti‑inflammatory tilt, tobacco fuels a chronic pro‑inflammatory state: higher IL‑1β, IL‑6, and C‑reactive protein (CRP). This persistent inflammation wears down tissues and predisposes to auto‑immune flare‑ups.
4. Diminished Adaptive Immunity
Smoking cuts IgA levels in mucosal secretions by roughly 25%, weakening the first line of defense in the respiratory tract. T‑cell proliferation after antigen exposure is also slower, making vaccines less effective.
Side‑by‑Side: Alcohol vs. Tobacco on Key Immune Markers
| Immune Aspect | Alcohol | Tobacco |
|---|---|---|
| Gut Barrier Integrity | Increased permeability, endotoxin leak | Minor effect; focus on lung barrier |
| White‑Blood‑Cell Count | -30% neutrophils/monocytes (chronic) | +10% neutrophils (reactive) but ↓ function |
| Phagocytic Activity | Reduced by ~35% | Reduced by ~40% in alveolar macrophages |
| Cytokine Profile | Shift toward IL‑10 (anti‑inflammatory) | Elevated IL‑1β, IL‑6, CRP (pro‑inflammatory) |
| Antibody Production | -20% after binge episodes | -15% IgA in mucosa |
| Vaccine Response | Reduced seroconversion ~10% | Reduced seroconversion ~15% |
Long‑Term Health Fallout
When the immune system stays compromised, the body pays a price:
- Higher infection rates: chronic drinkers are 2-3× more likely to develop pneumonia; smokers face a 4× risk of tuberculosis activation.
- Slower wound healing: collagen synthesis drops, leading to longer scar formation.
- Poor vaccine efficacy: flu and COVID‑19 vaccines generate weaker antibody titres in both groups.
- Elevated cancer risk: impaired immune surveillance allows mutated cells to escape detection.
- Auto‑immune flare‑ups: oxidative stress from tobacco can trigger diseases like rheumatoid arthritis.
How to Reboot Your Immune Defenses
Good news: the immune system is remarkably resilient. Here’s a roadmap you can start today.
- Cut the source: aim for ≤1 drink per day (women) or ≤2 (men). For tobacco, consider nicotine‑replacement therapy or a structured quit‑plan.
- Re‑hydrate & restore gut health: probiotic‑rich foods (yogurt, kefir), fiber, and plenty of water help seal the gut barrier.
- Boost antioxidant intake: berries, leafy greens, and vitaminC combat oxidative stress from any remaining smoke exposure.
- Prioritize sleep: 7-9hours restores cytokine rhythms and increases natural killer cell activity.
- Stay active: moderate exercise (30minutes, 5days a week) raises neutrophil circulation and improves vaccine response.
- Monitor your health: regular blood work (CBC, CRP) can flag lingering inflammation.
Within weeks of quitting, you’ll notice clearer skin, better stamina, and a measurable uptick in immune markers.
Frequently Asked Questions
Can occasional drinking still harm my immune system?
Yes, even a single binge (5+ drinks) can temporarily suppress neutrophil function for up to 24hours. Regular moderate drinking (1‑2 drinks daily) has a milder but still measurable impact on gut permeability.
Does vaping affect immunity the same way as cigarettes?
Vaping introduces fewer tar particles but still delivers nicotine and oxidative chemicals. It reduces macrophage activity by about 20%, so the immune‑impairing effect is present, though slightly less severe than traditional smoke.
Will quitting improve my response to the flu vaccine?
Studies show that people who quit smoking for at least 3months achieve a 10‑15% rise in antibody titres after flu vaccination, matching non‑smokers. Alcohol reduction yields a similar 8‑12% improvement.
How long does it take for gut permeability to normalize after I stop drinking?
Most research indicates that within 2‑4weeks of abstinence, tight‑junction proteins recover and endotoxin levels drop to baseline, especially when paired with a high‑fiber diet.
Are there any supplements that can help repair immune damage caused by alcohol or tobacco?
Zinc (30mg), vitaminD (2000IU) and omega‑3 fatty acids have the strongest evidence for boosting innate immunity and reducing inflammation. They work best alongside lifestyle changes rather than as a standalone fix.









Shawna B
30 Sep 2025 at 01:20I just quit smoking and my colds are way less bad. Took 3 weeks but my lungs feel lighter.