When a patient is on a medication with a narrow therapeutic index-like digoxin, vancomycin, or lithium-getting the dose right isn’t just important. It’s life-or-death. Too little, and the drug doesn’t work. Too much, and it can cause toxicity, organ damage, or even death. That’s why therapeutic drug monitoring (TDM) exists: to make sure the drug level in the blood stays in the safe, effective zone. But here’s the catch: if the lab test itself is flawed, the whole system fails. That’s where confirming the lab’s monitoring process comes in.
Why Lab Verification Isn’t Optional
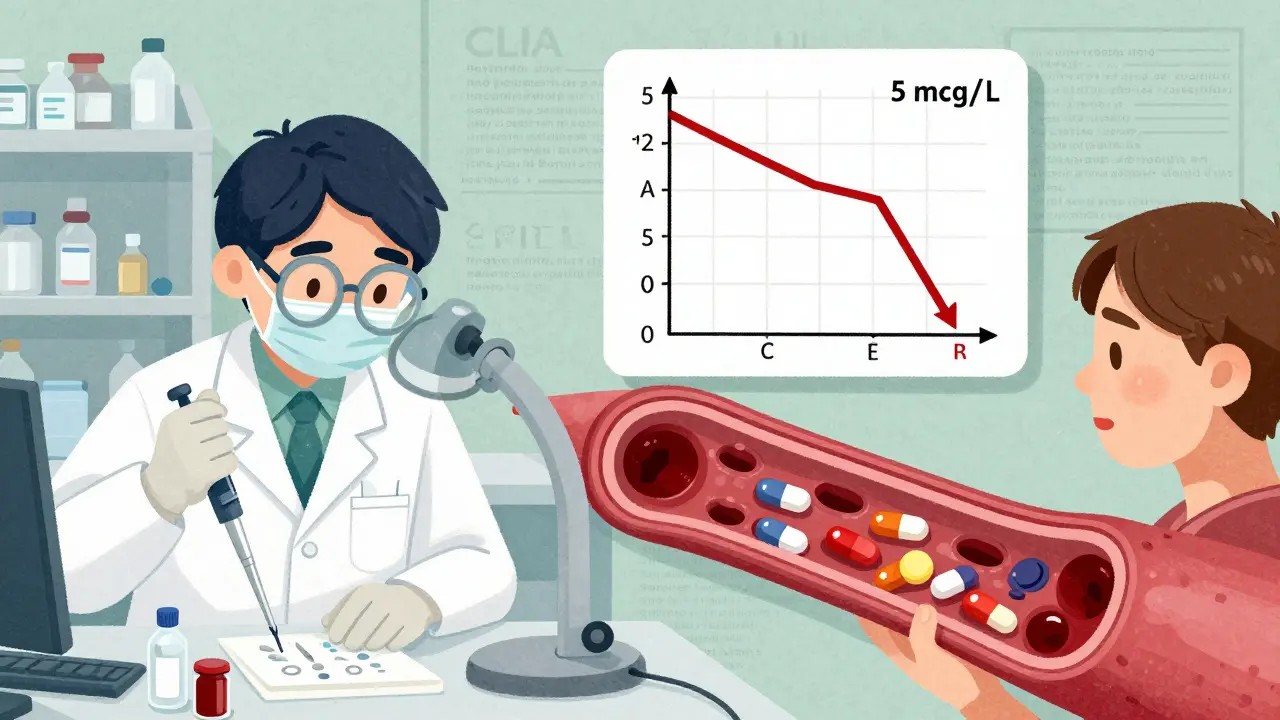
Many providers assume that if a lab says it runs a test for tacrolimus or carbamazepine, the result is trustworthy. That’s a dangerous assumption. Clinical labs don’t just plug in a machine and start reporting numbers. Every test must go through verification or validation before it’s used on patients. Under CLIA ’88 regulations, this isn’t a suggestion-it’s the law. Failure to comply can cost a lab $7,500 per violation, but more importantly, it puts patients at risk. A 2021 FDA review found that 32% of recalls for therapeutic drug monitoring tests were due to poor verification of cross-reactivity. For example, some digoxin immunoassays react not just to digoxin, but to its metabolites or even unrelated drugs like spironolactone. If the lab doesn’t test for this, a patient might be told their level is “normal” when it’s actually dangerously high. That’s not a lab error-it’s a system failure.Verification vs. Validation: Know the Difference
Not all lab tests are created equal. There are two paths to ensure accuracy:- Verification is for tests that already have FDA clearance-like most common TDM assays. The lab checks if the test performs as the manufacturer claims. This takes about 80 hours and costs $2,500-$5,000 per test.
- Validation is for lab-developed tests (LDTs), like those for clozapine metabolites, where no FDA-cleared test exists. This requires full performance assessment: precision, accuracy, sensitivity, interference testing, and more. It takes 120+ hours and costs $7,500-$15,000.
The 9-Step Verification Process (Simplified)
You don’t need to run the lab, but you should know what’s happening behind the scenes. Here’s how labs verify a test:- Plan it out - Define what performance standards will be used (based on CLSI EP15-A3 guidelines).
- Get approval - The lab director must sign off before any testing begins.
- Run the tests - At least 20 replicates over 5 days to check precision. Use reference materials to check trueness.
- Test for interference - Add common drugs like ibuprofen, acetaminophen, or antibiotics to samples. See if they throw off the result. For immunosuppressants, test against 12+ metabolites.
- Check the range - The test must accurately measure from below the minimum therapeutic level to above the maximum. For vancomycin, that’s 5-80 mcg/mL. For digoxin, it’s 0.5-4.0 ng/mL.
- Confirm linearity - The result must be proportional across the entire range. R² must be ≥0.99.
- Document everything - SOPs, raw data, calculations, and deviations.
- Train staff - At least 40-60 hours of training on the new protocol.
- Implement and monitor - After launch, track results for 30 days to catch hidden issues.
What You, as a Provider, Should Ask
You don’t need to run the lab. But you do need to know if the lab you’re using is doing it right. Here’s what to ask:- “Is this test FDA-cleared or lab-developed?” - If it’s lab-developed, ask if they’ve done full validation.
- “What’s the lower limit of quantitation for this drug?” - If they can’t tell you, they might not be detecting sub-therapeutic levels.
- “Have you tested for interference from common medications?” - Especially for drugs like carbamazepine, phenytoin, or immunosuppressants.
- “Do you report measurement uncertainty?” - Reputable labs include this. If they don’t, it’s a red flag.
- “What’s your turnaround time?” - If results take more than 48 hours for a critical drug like vancomycin, you might be missing the window for adjustment.
Follow-Up: What to Do After You Get the Result
Getting the lab result is just step one. The real work starts now.- Compare to therapeutic range - Don’t rely on the lab’s reference range. Use published guidelines. For example, the therapeutic range for lithium is 0.6-1.0 mmol/L. Anything above 1.2 is toxic.
- Check timing - Was the blood drawn at the right time? For most drugs, it’s peak or trough. Vancomycin should be drawn just before the next dose. Digoxin should be drawn 6-8 hours after the last dose.
- Correlate with clinical status - Is the patient still having seizures? Are they dizzy? Nauseous? A “normal” level doesn’t mean the drug is working if the patient is deteriorating.
- Adjust and retest - Don’t wait a month to recheck. For drugs like vancomycin, retest within 48-72 hours after a dose change. For lithium, wait 5-7 days.
- Document the rationale - Why did you increase the dose? Why did you hold it? This protects you and informs future providers.

Technology Is Helping-But Not Replacing Human Judgment
New EHR systems now auto-flag out-of-range TDM results. Epic’s system, now in 45% of U.S. hospitals, can alert you if a vancomycin level is trending upward or if a patient has multiple drugs that interfere with each other. But alerts aren’t foolproof. One hospital reported that 60% of their TDM alerts were false positives because the system didn’t account for timing or patient weight. The best systems combine tech with protocols: if a level is flagged, the EHR prompts you to check the timing, the patient’s renal function, and recent drug changes. That’s the future. But right now, you’re still the final check.Common Pitfalls and How to Avoid Them
Here’s what goes wrong-and how to stop it:- Assuming all labs are equal - Community hospitals often use cheaper, less accurate platforms. Academic centers use more precise methods. Ask which platform the lab uses.
- Ignoring sample timing - A trough level drawn too early can look falsely low. Always confirm when the sample was taken.
- Not checking for drug interactions - Antibiotics like ciprofloxacin can raise tacrolimus levels by 50%. Always review the med list.
- Delaying follow-up - Waiting a week to adjust a dose on a narrow-therapeutic-index drug is negligent. Act fast.
- Not documenting changes - If you change a dose based on a lab result, write it down. If you don’t, someone else might repeat the same mistake.
Final Thought: Your Role Is Critical
You’re not just prescribing. You’re managing a complex system that includes labs, EHRs, pharmacists, and patients. The lab result is only as good as the process behind it. If you don’t ask questions, you’re trusting automation to protect your patient. But automation doesn’t think. It doesn’t notice a patient who’s vomiting and dehydrated. It doesn’t know if the sample was drawn from the wrong arm. The best providers don’t just read lab results. They understand how they were made. They know when to push back. They follow up. They document. And they never assume.What’s the difference between verification and validation in lab testing?
Verification is used for FDA-cleared tests and confirms the test performs as the manufacturer claims. It’s faster and cheaper. Validation is used for lab-developed tests (LDTs) and requires full performance testing-precision, accuracy, interference, and more. It’s more time-consuming and expensive but necessary when no FDA-cleared test exists.
Which medications require therapeutic drug monitoring?
Common ones include lithium, vancomycin, digoxin, carbamazepine, phenytoin, cyclosporine, tacrolimus, and valproic acid. These drugs have narrow therapeutic windows-small changes in dose can cause toxicity or treatment failure.
How often should drug levels be checked?
It depends on the drug and patient. For vancomycin, check after the third dose and after any dose change. For lithium, wait 5-7 days after a dose change. For chronic stable patients, monthly checks may be enough. Always follow clinical guidelines and patient response.
Can lab results be wrong even if they’re in range?
Yes. Interference from other drugs, improper sample timing, or poor test validation can cause falsely high or low results. A patient can have a level in the “normal” range but still be toxic if the test isn’t specific enough. Always correlate with clinical signs.
What should I do if I suspect a lab error?
Don’t ignore it. Contact the lab and ask if they verified the test, checked for interference, and confirmed the lower limit of quantitation. Request a repeat sample using a different method or lab. If the result is still questionable, treat the patient based on symptoms, not the number.
Are there tools to help track medication monitoring?
Yes. Many EHRs now have built-in TDM modules that flag out-of-range levels, suggest dose adjustments, and remind you when to recheck. Epic and Cerner offer these. But they’re only as good as the data you input. Always verify timing, clinical context, and patient history before acting.



Brenda King
22 Jan 2026 at 03:00Just saw a case where a patient’s digoxin level came back 'normal' but they were crashing-turns out the lab didn’t test for digitoxin cross-reactivity. Scary stuff. Always ask about interference. 🤕