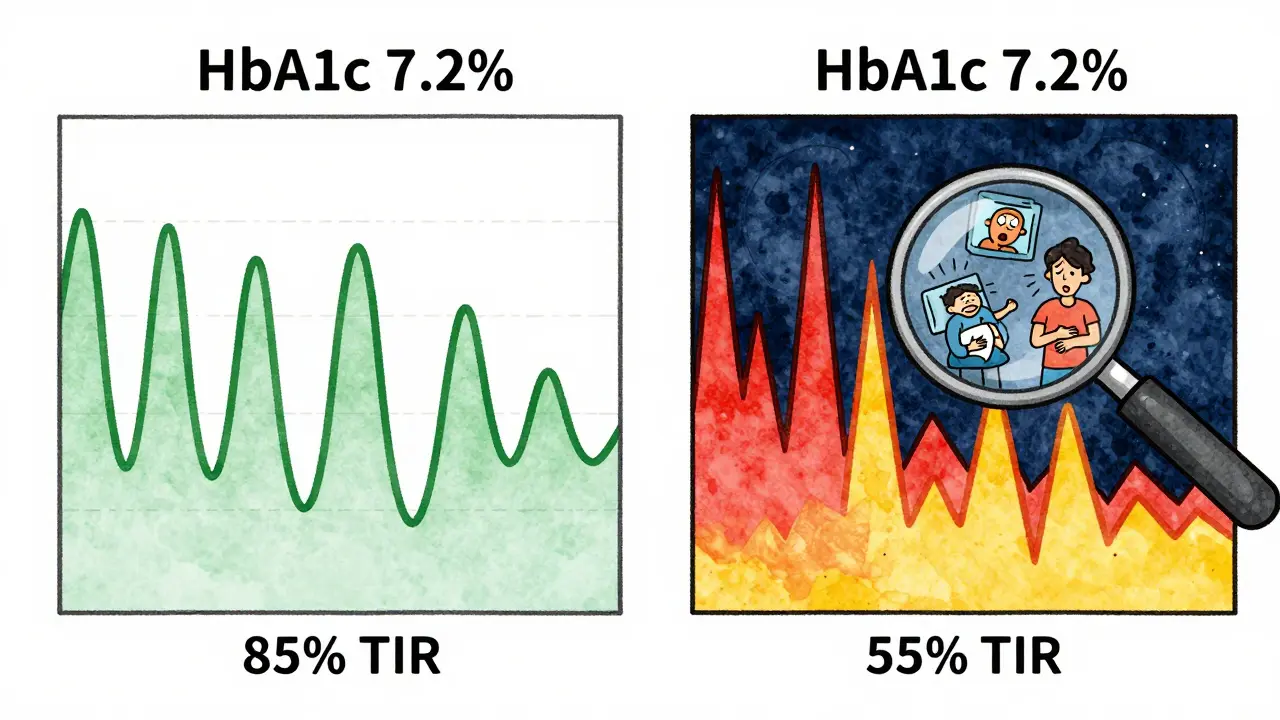
Most people with diabetes know their HbA1c number. It’s the number doctors check every three months - a single number that’s supposed to tell you how well your blood sugar is controlled. But here’s the problem: two people can have the exact same HbA1c of 7%, and one could be spending 20 hours a day in range while the other is crashing into hypoglycemia at 3 a.m. and soaring past 250 mg/dL after lunch. HbA1c hides the chaos. That’s where time in range changes everything.
What Exactly Is Time in Range?
Time in range, or TIR, is simply the percentage of time your blood glucose stays between 70 and 180 mg/dL (3.9-10.0 mmol/L). It’s measured by a continuous glucose monitor (CGM), a small sensor worn on your arm or belly that checks your glucose every 1 to 5 minutes. Over 14 days, that’s over 1,300 readings - not one average, but a full story of your day.
The goal? Spend at least 70% of your day - about 17 hours - in that sweet spot. That’s the target set by the American Diabetes Association (ADA) in their 2025 Standards of Care and backed by international experts. If you hit that, you’re likely keeping your HbA1c around 7%, but with far fewer dangerous spikes and drops.
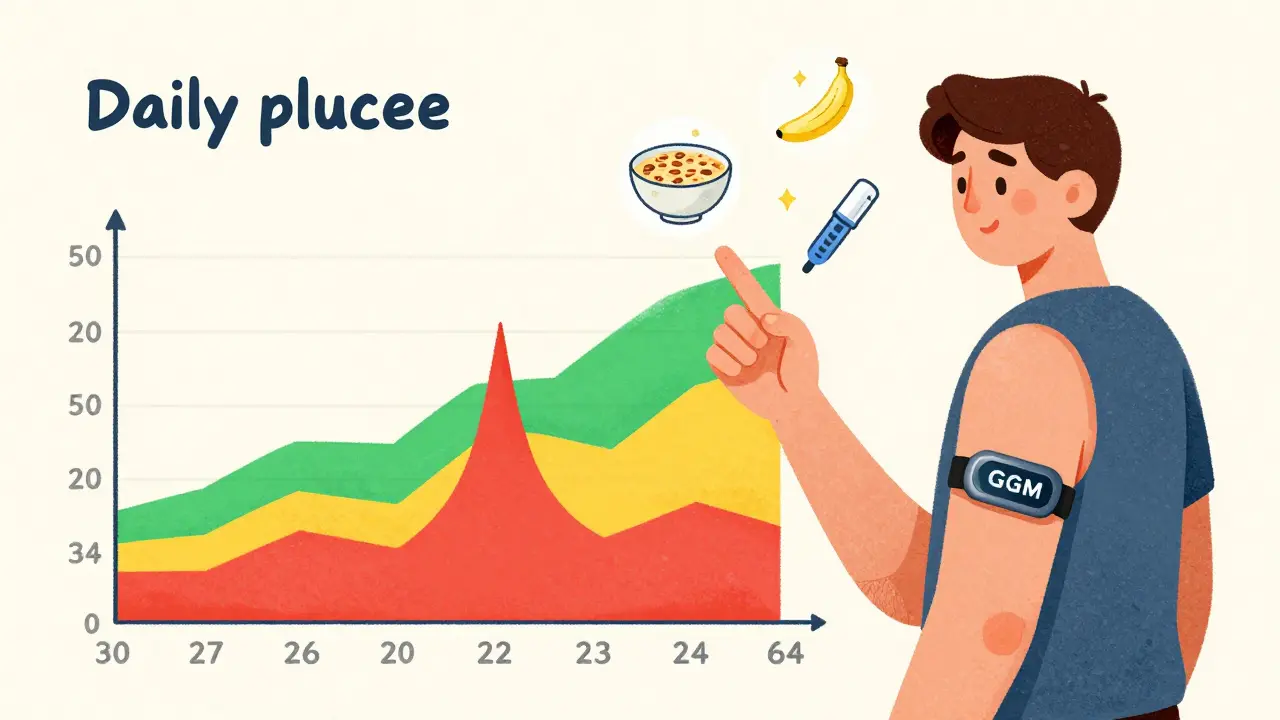
It’s not just about the number. TIR shows you when your glucose is high or low. Did your sugar drop after walking? Did that ‘healthy’ oatmeal spike you into the 200s? That’s the kind of detail HbA1c can’t touch.
Why TIR Beats HbA1c for Daily Control
HbA1c is like reading the last page of a book. You know how it ended, but you have no idea what happened in chapter 3. TIR is reading the whole thing.
Take two patients: both with an HbA1c of 7.2%. One has a TIR of 85%. They’re stable. They rarely go below 70 or above 180. The other has a TIR of 55%. Their glucose swings wildly - low at night, high after meals. Even though their averages are the same, the second person is at much higher risk for complications. They’re living with constant stress on their body, even if the lab report says they’re ‘doing fine.’
Studies show TIR is more closely linked to real-world outcomes than HbA1c alone. Lower TIR means more time spent in hypoglycemia - which increases risk of falls, confusion, even heart problems. Higher TIR means less time in hyperglycemia - which reduces long-term damage to kidneys, eyes, and nerves.
And here’s the kicker: TIR can improve without changing your HbA1c. You can lower your spikes and lows without moving your average much. That’s a win. You’re not just managing numbers - you’re managing your life.
The Other Metrics That Matter With TIR
TIR doesn’t work alone. It’s part of a trio:
- Time Below Range (TBR): Time spent under 70 mg/dL. Aim for under 4% (less than 1 hour/day). If you’re hitting below 54 mg/dL, that’s severe hypoglycemia - and you need to act.
- Time Above Range (TAR): Time over 180 mg/dL. Less than 25% is ideal. If you’re spending 40% of your day above target, your insulin or meds aren’t matching your food or activity.
- Glucose Variability: Measured by coefficient of variation (CV). A CV under 36% means your glucose isn’t bouncing around too much. High variability = more stress on your body.
Some people aim for an even tighter range - 70 to 140 mg/dL - especially if they’re researching physiological norms or have very good control. But for most, 70-180 is the realistic, safe target.
How CGM Makes TIR Possible
Before CGM, we relied on fingersticks - maybe 4 to 8 checks a day. That’s a snapshot. CGM gives you a movie. It tracks trends, not just numbers. You can see if your glucose is rising fast after breakfast or dipping slowly overnight.
Modern sensors like Dexcom G7, Abbott Libre 3, or Medtronic Guardian work for up to 14 days without calibration. They sync with apps that show your TIR as a color-coded bar: green for in range, yellow for high, red for low. It’s intuitive. You don’t need to be a scientist to see if you’re spending too much time in red.
But it’s not magic. You need to wear it. The 2019 International Consensus says you need at least 70% active wear time over 14 days to get reliable data. That means no taking it off for showers or workouts unless you’re ready to lose half your data.
And yes - sensors can be uncomfortable. They itch. They peel. Sometimes they give weird readings. But most users say the trade-off is worth it. One man in Leeds told me he finally understood why he felt so tired after lunch - his CGM showed his glucose spiked to 220 after eating a banana with peanut butter. He swapped the banana for berries. His TIR jumped from 58% to 74% in two weeks.
Who Should Use TIR? It’s Not Just for Insulin Users Anymore
For years, CGM was seen as something only people on insulin needed. That changed in 2025. The ADA now says any adult with type 2 diabetes on glucose-lowering meds - even metformin or GLP-1 agonists - should consider CGM if they’re not hitting their goals.
Why? Because you don’t need insulin to have dangerous highs and lows. People on SGLT2 inhibitors can get hypoglycemia. People on sulfonylureas can crash overnight. And many with type 2 diabetes don’t even know they’re having silent highs until their HbA1c jumps.
Studies show that non-insulin users who start CGM improve their TIR, lower their HbA1c, and report better quality of life. One 2024 trial found that people on metformin and a GLP-1 drug who used CGM for 12 weeks reduced their time above range by 30% - without changing their meds.
This isn’t luxury. It’s precision medicine. If your doctor still says CGM is only for insulin users, they’re working off outdated guidelines.
Getting Started With TIR: What You Need to Do
Here’s how to make TIR work for you:
- Get a CGM: Ask your doctor for a prescription. In the UK, NHS access is expanding, but private options like Abbott Libre are widely available. Insurance coverage in the US has improved dramatically since 2023.
- Wear it for 14 days: Don’t skip days. Even if you think you know your patterns, the data will surprise you.
- Track your habits: Write down meals, exercise, stress, sleep, and medication times. Don’t rely on memory.
- Review with your care team: Bring your CGM report to your next appointment. Ask: ‘Where am I spending too much time out of range?’
- Adjust, don’t guess: If your glucose spikes after pasta, try swapping half the pasta for lentils. If you drop overnight, talk about your evening insulin or bedtime snack.
Most people need one or two visits to learn how to read the graphs. After that, it becomes second nature. You start noticing patterns: ‘I always go high after coffee with cream’ or ‘Walking after dinner cuts my spike by half.’ That’s power.

Barriers - And How to Overcome Them
Cost and access are still real issues. In the UK, NHS access varies by region. In the US, insurance denials still happen. But the tide is turning. Medicare coverage for CGM in type 2 diabetes jumped from 15% in 2019 to 42% in 2023. Companies like Abbott have slashed prices on Libre sensors. Some pharmacies now offer them for under £50 per 14-day sensor.
Another barrier? Overwhelm. Seeing a graph full of red and yellow can feel discouraging. That’s why education matters. Organizations like ADCES offer free training on interpreting CGM data. Don’t try to fix everything at once. Pick one target: ‘I want to reduce my morning highs.’ Focus there. Small wins build confidence.
What’s Next for Time in Range?
The future is personalized. AI tools are starting to analyze your TIR data and suggest changes - ‘Try moving your dinner to 7 p.m. instead of 8:30 p.m. Your glucose drops 30 points.’
Researchers are also looking at ‘time in tight range’ (70-140 mg/dL) as a new goal, especially for younger patients or those with prediabetes. The idea? The closer you get to a non-diabetic glucose pattern, the better your long-term health.
And the data keeps getting stronger. The T1D Exchange Registry and other large studies are now tracking thousands of people over years to link TIR directly to kidney disease, retinopathy, and heart events. We’re moving from correlation to causation.
Time in range isn’t a trend. It’s the new foundation of diabetes care. It turns vague averages into actionable insights. It gives you back control - not just over your numbers, but over your life.
Final Thought: It’s Not About Perfection
You don’t need 100% time in range. That’s unrealistic. Even people without diabetes spend 10-15% of their day outside 70-180 mg/dL. The goal is to reduce the extremes. To spend less time in the red. To avoid the crashes. To feel steady.
If your TIR goes from 50% to 65%, that’s progress. If you cut your nighttime lows by half, that’s a win. TIR doesn’t demand perfection. It rewards awareness. And that’s the biggest gift of all.






Rob Webber
30 Jan 2026 at 07:37This whole TIR thing is just another way for Big Med to sell you more sensors and apps. HbA1c has worked for 70 years. Now you need a $100 sensor just to know if your blood sugar is okay? I’ve been diabetic for 22 years and I’ve never needed a movie-I’ve been fine with four fingersticks a day.