Hypoglycemia Risk Calculator for Diabetes Medications
Alcohol and Diabetes Medication Risk Assessment
Drinking alcohol while taking diabetes medication isn’t just a bad idea-it can be dangerous, even life-threatening. If you’re on insulin, sulfonylureas, or metformin, alcohol doesn’t just add empty calories. It interferes with your body’s ability to keep blood sugar stable and puts extra strain on your liver. And the worst part? You might not even realize you’re in danger.
Why Alcohol Lowers Blood Sugar (Even When You Don’t Think It Should)
Your liver does two big jobs at once: it stores sugar when you’ve eaten too much, and it releases sugar when your levels drop. When you drink alcohol, your liver drops everything to deal with the toxin. It stops releasing glucose into your bloodstream. That’s fine if you’ve just eaten a meal. But if you’re fasting, skipping dinner, or exercising after a drink, your blood sugar can crash-fast.
This is especially risky if you take insulin or sulfonylureas like glipizide or glyburide. These drugs push your pancreas to make more insulin, which lowers blood sugar. Alcohol shuts down your liver’s backup system. The result? Double trouble. Blood sugar can drop below 70 mg/dL within an hour-and stay low for hours after your last sip.
And here’s the hidden danger: the signs of low blood sugar-dizziness, confusion, slurred speech, sweating, shakiness-look exactly like being drunk. If you pass out after a few drinks, someone might think you’re just intoxicated. They won’t know you need glucose, not more alcohol. That delay can lead to seizures, coma, or even death.
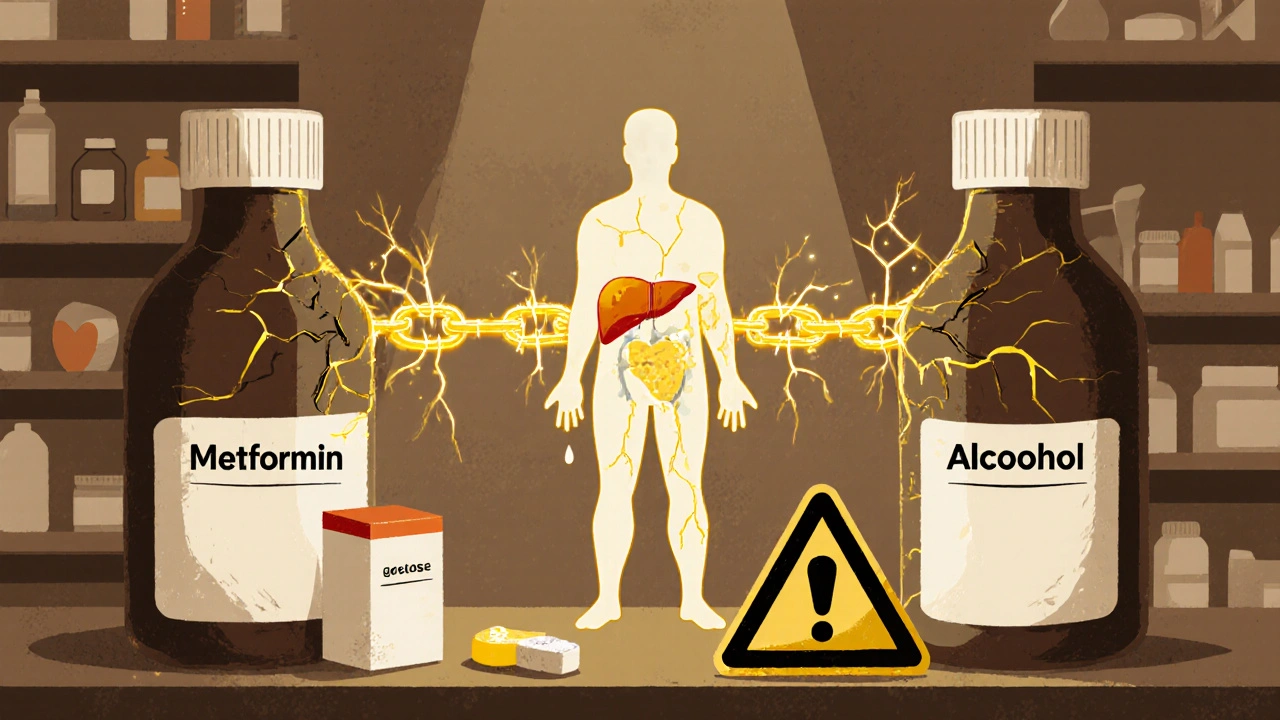
Metformin and Alcohol: A Silent Strain on the Liver
Metformin is one of the most common diabetes pills. It’s generally safe-but mixing it with alcohol ups the risk of something called lactic acidosis. It’s rare, but deadly. This happens when your body builds up too much lactic acid, usually because your liver and kidneys can’t clear it properly.
Alcohol slows down how fast your liver processes metformin. At the same time, alcohol itself stresses the liver. Over time, heavy drinking can cause fatty liver disease, inflammation, or even cirrhosis. If your liver is already damaged, metformin can build up in your system, increasing the chance of serious side effects.
Even moderate drinking-two drinks a night-can make metformin side effects worse. Nausea, stomach cramps, diarrhea, and bloating become more intense. Many people think these are just "gut issues" and ignore them. But when alcohol is involved, these symptoms could be early warning signs of something more serious.
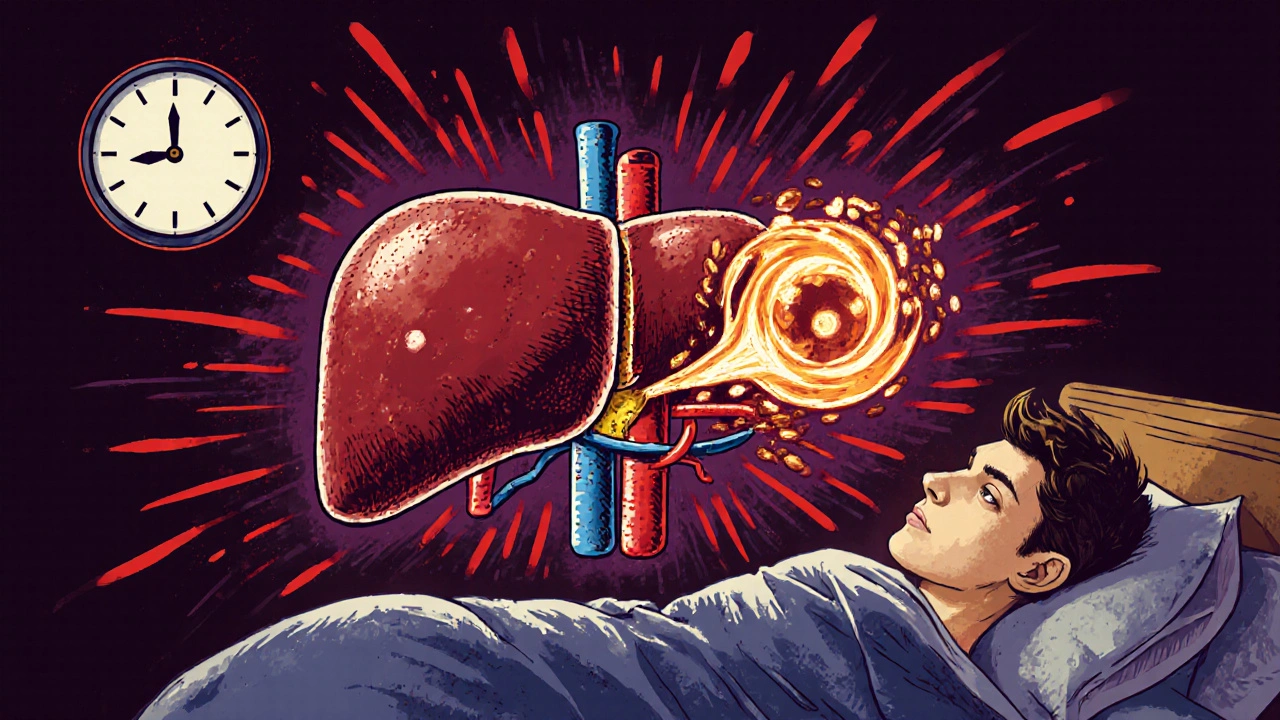
Delayed Hypoglycemia: The Nighttime Trap
Most people think the danger is right after drinking. But the real threat comes hours later. Alcohol can cause low blood sugar up to 12-24 hours after your last drink, especially if you drank on an empty stomach or exercised afterward.
That’s why so many people with diabetes wake up in the middle of the night confused, sweaty, or with a pounding headache. They check their meter and see a reading of 52 mg/dL. They didn’t eat after drinking. They didn’t set an alarm. They didn’t tell anyone they were drinking. By the time they realize what’s happening, it’s too late.
Continuous glucose monitors (CGMs) like the Dexcom G7 or FreeStyle Libre 3 can help. They show trends, not just numbers. If your glucose drops steadily through the night, even if you’re asleep, the alarm will wake you. But if you don’t use one, you’re flying blind.

What to Drink (and What to Avoid)
Not all alcoholic drinks are equal when you have diabetes.
- Best choices: Dry white wine, light beer, or spirits (vodka, gin, whiskey) mixed with soda water and lime. These have minimal sugar and carbs.
- Avoid: Sweet cocktails, margaritas, piña coladas, regular soda mixers, juice, and liqueurs. A single margarita can have 30+ grams of sugar-that’s more than a candy bar.
- Watch portion sizes: One drink means 12 oz of beer, 5 oz of wine, or 1.5 oz of hard liquor. Anything more counts as multiple drinks.
And never drink on an empty stomach. Always eat a meal or snack with carbs-like whole grain toast, fruit, or a small bowl of oatmeal-before you start drinking. Eating slows down alcohol absorption and gives your liver something to work with besides just detoxing.
Who Should Skip Alcohol Completely?
Some people with diabetes should avoid alcohol entirely:
- Those with a history of severe hypoglycemia or hypoglycemia unawareness
- People with liver disease, including fatty liver or cirrhosis
- Anyone taking metformin who drinks more than 1-2 drinks per week
- Those with nerve damage (neuropathy)-alcohol makes it worse
- Women who are pregnant or trying to conceive
Heavy drinking is defined as more than 15 drinks a week for men or 8 for women. That level of alcohol use increases insulin resistance, damages the pancreas, and raises blood pressure-all bad news for diabetes control.
Practical Safety Tips
If you choose to drink, follow these steps:
- Check your blood sugar before you drink. Don’t drink if it’s below 100 mg/dL.
- Eat a carb-containing meal or snack. Don’t skip this step, even if you’re not hungry.
- Wear a medical ID. It should say "Diabetic" and list your medications. In an emergency, this saves lives.
- Tell someone you’re with. Let a friend know you have diabetes. Ask them to watch for signs of low blood sugar.
- Set an alarm. If you drank after dinner, set a reminder to check your blood sugar at 2 a.m. and again in the morning.
- Carry fast-acting glucose. Glucose tablets, juice boxes, or candy should be with you at all times when drinking.
Many people think, "I only have one drink." But one drink can be enough to trigger a dangerous drop, especially if you’re on insulin or metformin. There’s no "safe" amount-only safer choices and better preparation.
What Doctors Say (And Don’t Say)
A 2021 study found that less than half of primary care doctors regularly ask their diabetic patients about alcohol use. That’s a huge gap. Your doctor should know if you drink-not to judge you, but to adjust your meds, warn you about risks, or help you find safer alternatives.
The American Diabetes Association doesn’t ban alcohol. Instead, they say: "It’s personal." Your risk depends on your meds, your liver health, your history of low blood sugar, and how much you drink. There’s no one-size-fits-all rule.
If you’re unsure, ask your doctor or diabetes educator these three questions:
- "Does my medication increase my risk of low blood sugar with alcohol?"
- "Is my liver healthy enough to handle even small amounts?"
- "Should I adjust my insulin or medication dose if I plan to drink?"
Most people get a simple answer: "Don’t drink." But if you’re careful, informed, and prepared, some can drink occasionally without disaster. The key isn’t guilt-it’s awareness.
What’s New in 2025?
Research is moving fast. In 2023, the Joslin Diabetes Center began a 12-month study tracking how moderate alcohol use affects liver function in people on metformin. Early data suggests even moderate drinking can cause subtle liver changes over time-even in people who don’t have fatty liver disease.
CGM companies are also working on algorithms that flag patterns linked to alcohol. In the next year, your glucose monitor might say: "Your levels dropped sharply after drinking. Consider reducing intake or checking more often."
For now, the best tool you have is your own body. Learn your signs. Track your habits. Talk to your care team. And remember: alcohol doesn’t care if you have diabetes. Your body does. Protect it.
Can I drink alcohol if I take metformin?
You can, but it’s risky. Metformin and alcohol both stress the liver. Together, they increase the chance of lactic acidosis-a rare but serious condition. Even one or two drinks can make nausea, cramps, and fatigue worse. If you have liver problems, nerve damage, or a history of low blood sugar, avoid alcohol entirely. If you choose to drink, stick to one drink occasionally, always eat food first, and check your blood sugar before bed.
Why does alcohol cause low blood sugar hours after drinking?
Your liver stops releasing glucose to focus on breaking down alcohol. This can last for hours-even after you’ve stopped drinking. If you didn’t eat, your body has no backup sugar source. That’s why low blood sugar often hits at night or the next morning. It’s not the alcohol itself lowering sugar-it’s your liver being too busy detoxifying to help you.
What’s the safest alcohol to drink with diabetes?
The safest options are dry wine (like Sauvignon Blanc), light beer, or spirits (vodka, gin, whiskey) mixed with soda water and lime. Avoid sugary mixers like juice, soda, or syrups. A single drink should be 5 oz of wine, 12 oz of light beer, or 1.5 oz of hard liquor. Always count it as one drink-even if you pour more.
Can alcohol make diabetes worse over time?
Yes. Heavy drinking (more than 15 drinks a week for men, 8 for women) increases insulin resistance, raises triglycerides, damages the pancreas, and can lead to fatty liver disease or cirrhosis. All of this makes blood sugar harder to control. Even moderate drinking can worsen nerve damage and increase blood pressure. The long-term risks often outweigh any small heart benefits.
Should I check my blood sugar after drinking?
Always. Check before you start, during if you’re out, and again before bed-even if you feel fine. Alcohol can cause a drop up to 24 hours later. If you use a CGM, watch for a steady downward trend overnight. Set an alarm to check at 2 a.m. if you drank after dinner. Never assume you’re safe just because you felt okay at first.
What should I do if I feel dizzy or confused after drinking?
Don’t assume you’re just drunk. Check your blood sugar immediately. If it’s below 70 mg/dL, treat it with 15 grams of fast-acting carbs: 4 glucose tablets, ½ cup of juice, or 1 tablespoon of honey. Wait 15 minutes and check again. If you can’t check or don’t have access to sugar, call for help. Tell someone you have diabetes. Symptoms of low blood sugar and intoxication look the same-don’t wait for someone else to figure it out.
Is it safe to drink alcohol if I use insulin?
It’s possible, but high-risk. Insulin lowers blood sugar, and alcohol shuts down your liver’s ability to raise it. The combination can cause sudden, severe hypoglycemia. If you use insulin, you should only drink occasionally, always with food, and never without checking your levels. Many people on insulin choose to avoid alcohol entirely to reduce the danger. Talk to your diabetes educator about your specific plan.
Can alcohol interact with other diabetes medications besides metformin and insulin?
Yes. Sulfonylureas like glipizide and glyburide carry the same hypoglycemia risk as insulin. Even newer drugs like DPP-4 inhibitors or GLP-1 agonists can interact indirectly-alcohol can worsen nausea or stomach upset, which are already side effects. Always check your medication’s warning label and ask your pharmacist or doctor if alcohol is safe with your specific drugs.








Shivam Goel
26 Nov 2025 at 11:29Alcohol + metformin = lactic acidosis risk? Yeah, and it’s not just theoretical-I saw a guy in the ER last year with a lactate of 12. He thought one whiskey was fine. He didn’t know his liver was already fatty from years of weekend binges. Now he’s on dialysis. Don’t be him.