When your breathing gets tight every spring, or you wake up gasping after a dusty day, it’s not just a cold-it could be allergic asthma. This isn’t just bad allergies with wheezing. It’s your immune system overreacting to things like pollen, dust mites, or cat dander, turning them into triggers that tighten your airways and make it hard to breathe. About 60% of adults and over 80% of children with asthma in the U.S. have this type. The good news? You can take control-not just with inhalers, but by changing your environment and even retraining your immune system.
What Really Triggers Allergic Asthma?
Allergic asthma doesn’t happen randomly. It’s tied to specific allergens that your body sees as threats-even though they’re harmless. The most common ones are airborne and vary by season and location.
Tree pollen hits hardest in early spring-February to April-with peak levels in March. Grass pollen takes over in late spring and early summer, especially June, when counts can jump to 50-100 grains per cubic meter. Then comes ragweed in late summer, often peaking in September with counts over 100 grains/m³. These aren’t just numbers-they’re real triggers. One study found emergency visits for asthma jumped 3.5 times during thunderstorms when ragweed spores burst open and spread deeper into lungs.
Indoors, the problem doesn’t stop. Dust mites thrive in bedding, carpets, and upholstered furniture when humidity is above 50%. In fact, 84% of U.S. homes have dust mite levels high enough to trigger reactions. Cat allergen (Fel d 1) is everywhere-even in homes without cats. It sticks to clothes, spreads through air vents, and lingers for months. Levels above 8 µg/g of dust are enough to cause symptoms in sensitive people. Dog allergen (Can f 1) is also common, found in 67% of homes.
Mold is another silent trigger, especially Alternaria. It grows in damp places like bathrooms and basements. When spore counts hit 500 per cubic meter, ER visits for asthma spike. And it’s not just about cleaning-it’s about controlling moisture. A 2022 study showed that keeping indoor humidity at 45% dropped dust mite allergens from 20 µg/g to just 0.5 µg/g.
How to Avoid Allergens-For Real Results
Avoiding allergens isn’t about occasional cleaning. It’s about building a system. Here’s what actually works, backed by research.
- Use allergen-proof covers on mattresses, pillows, and box springs. Brands like AllerZip Pro have been shown to reduce dust mite exposure by over 90%.
- Vacuum at least twice a week with a HEPA-filter vacuum. A Dyson V15 or similar model can pull out 42% more cat allergen than standard vacuums.
- Wash bedding weekly in water hotter than 130°F. Cold water won’t kill dust mites. Hot water cuts allergen levels by 90%.
- Keep indoor humidity between 30-50%. Use a hygrometer to monitor it. If it’s too high, a dehumidifier like the AprilAire 500M can drop levels fast.
- Keep windows closed when pollen counts exceed 9.7 grains/m³. Check local pollen forecasts daily. Apps like Pollen.com or the National Allergy Bureau provide real-time data.
- Wear an N95 mask when doing yard work. It cuts pollen exposure by 85%. Shower and change clothes right after coming inside-this reduces allergen transfer to your bed by 70%.
- Remove carpeting if possible. Hard floors are easier to clean and hold fewer allergens. If you have rugs, wash them monthly.
One user on Reddit tracked their progress: after installing allergen-proof covers, upgrading to a HEPA vacuum, and using a dehumidifier, their peak flow improved from 380 to 470 L/min over six months. That’s not luck-it’s science.

Immunotherapy: Rewiring Your Immune System
If avoidance isn’t enough, and medications like inhalers aren’t giving you full control, immunotherapy might be the next step. Unlike drugs that mask symptoms, immunotherapy changes how your body reacts to allergens-long-term.
There are two main types: subcutaneous (SCIT) and sublingual (SLIT). SCIT means regular allergy shots. You start with weekly injections of tiny amounts of the allergen, slowly increasing over 4-6 months until you reach a maintenance dose. Then you get shots monthly for 3-5 years. About 70-80% of people see major improvement after 12-18 months.
SLIT is the pill-or-drop version. You take a tablet (like Grastek for grass) or drops under your tongue daily. It’s less invasive, but you have to stick with it. In one trial, SLIT reduced asthma symptoms by 35% in dust mite-allergic patients-compared to just 15% with inhaled steroids alone.
It’s not instant. You won’t feel better overnight. But the payoff is big: a 2021 Cochrane review found immunotherapy reduces asthma medication use by up to 40%. And the benefits last. A 10-year follow-up study showed patients stayed symptom-free for years after stopping treatment.
There are downsides. SCIT can cause swelling or itching at the injection site. About 28% of users report mild reactions in the first year. SLIT often causes mouth or throat itching at first-78% of users feel it in the first month. But most get used to it. And serious reactions are rare when done under medical supervision.
Who Benefits Most from Immunotherapy?
Not everyone with allergic asthma needs it. But certain people see the biggest gains.
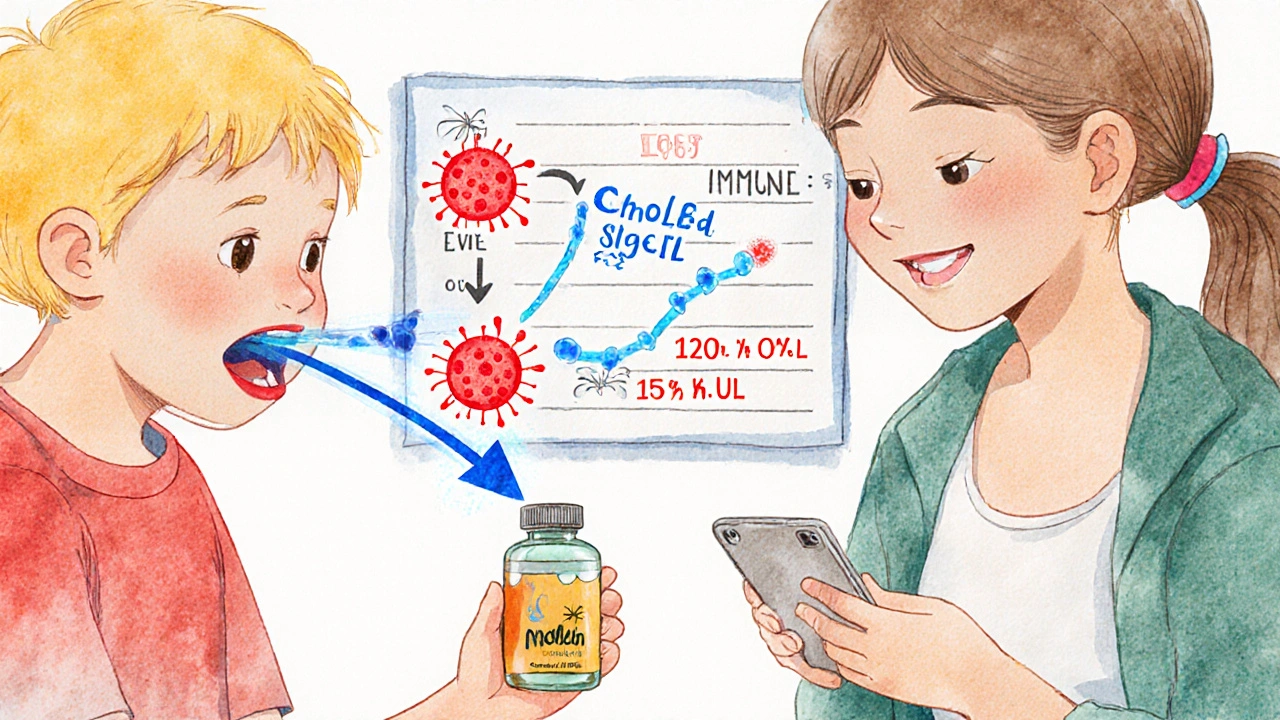
If you’re under 18 and have asthma triggered by one or two clear allergens-like dust mites or pollen-you’re a great candidate. Kids respond especially well. One 12-year-old with severe cat allergy had IgE levels drop from 120 to 15 kU/L after three years of immunotherapy. Their symptoms vanished. They stopped needing rescue inhalers.
Adults with moderate-to-severe asthma who rely on daily steroids also benefit. Studies show immunotherapy reduces flare-ups by 30-50% more than medication alone. It’s especially helpful if you’ve tried multiple inhalers and still struggle.
But if your asthma isn’t allergic-or if your triggers are too many (like dust, mold, pet, and pollen all at once)-immunotherapy might not help as much. Blood tests and skin prick tests can confirm if your asthma is IgE-driven. If your eosinophil count is above 300 cells/µL and your FeNO (fractional exhaled nitric oxide) is over 25 ppb, you’re likely a type 2 inflammatory responder-and immunotherapy will probably work.
Watch out for misdiagnosis. One expert warns that over 30% of people labeled as having allergic asthma actually have non-type 2 inflammation. They’re given expensive biologics (costing $30K-$40K a year) that don’t work. Proper testing is key.
What’s New in Allergic Asthma Treatment?
The field is moving fast. New tools are making diagnosis and treatment smarter.
There’s now a nasal sensor called Allergen Insight-FDA-approved in 2023-that detects airborne allergens as low as 0.1 µg/m³. It connects to your phone and alerts you when it’s unsafe to go outside. Another tool, AsthmaIQ, uses AI to predict flare-ups by combining pollen forecasts, your medication use, and even air quality data. It’s 92% accurate at predicting attacks.
Immunotherapy is getting faster, too. A new treatment called CAT-PAD cuts the build-up phase from six months to just eight weeks. And a pollen vaccine in Phase III trials showed 60% symptom reduction with only four doses a year.
Genetic testing is coming. A blood test for the GSDMB gene variant can now predict with 85% accuracy who will respond well to immunotherapy. That means fewer wasted treatments and better outcomes.
And the cost? In the U.S., Medicare covers 80% of immunotherapy under Part B. That’s a $18.90 copay per shot. In Europe, where healthcare is universal, nearly 28% of allergic asthma patients get immunotherapy-compared to just 15% in the U.S. More access means better long-term results.
What to Do Next
If you’re tired of relying on inhalers and still struggling to breathe:
- Track your symptoms for two weeks. Note when they get worse-after being outside? After vacuuming? Around pets?
- Get tested. Ask your doctor for a skin prick test or blood test for specific IgE antibodies. Don’t assume-you need proof.
- Start allergen avoidance. Change bedding, use a HEPA vacuum, control humidity. Do it now-it helps even if you don’t do immunotherapy yet.
- If avoidance isn’t enough, talk to an allergist about immunotherapy. Ask if you’re a candidate for SCIT or SLIT. Ask about cost, coverage, and expected timeline.
- Use new tools. Download a pollen app. Consider a hygrometer. If you’re tech-savvy, try AsthmaIQ.
Allergic asthma doesn’t have to control your life. With the right triggers identified, the right environment built, and the right treatment plan, you can breathe easier-not just today, but for years to come.
Can allergic asthma be cured?
There’s no permanent cure, but immunotherapy can lead to long-term remission. Many patients stop needing daily medications after 3-5 years of treatment. Studies show symptom control lasts for years after stopping therapy, especially if started early.
Is immunotherapy safe for children?
Yes. Immunotherapy is one of the most effective long-term treatments for children with allergic asthma. The American Academy of Allergy, Asthma & Immunology recommends it for kids as young as 5, especially if they have severe symptoms or multiple allergies. Sublingual tablets are often preferred for children because they’re easier to take than shots.
How long does it take to see results from allergen avoidance?
You may notice small improvements in a few weeks-like fewer nighttime coughs or less need for rescue inhalers. But full benefits, like improved lung function or reduced medication use, usually take 3-6 months of consistent effort. Patience and persistence matter.
Do air purifiers help with allergic asthma?
Yes, but only if they have a true HEPA filter. Standard air purifiers without HEPA don’t remove small allergens like dust mites or pet dander. A HEPA purifier can reduce airborne allergens by up to 90%. Place it in your bedroom for best results.
Can I still have pets if I have allergic asthma?
It’s possible, but challenging. Cat and dog allergens stick to surfaces and spread easily. If you keep a pet, keep them out of the bedroom, bathe them weekly, and use a HEPA air purifier. Some people with mild allergies tolerate pets better after starting immunotherapy. But if symptoms are severe, rehoming may be the best option.
Are there natural remedies that work for allergic asthma?
No proven natural remedies replace medical treatment. Honey, saline rinses, or herbal supplements may offer minor relief but don’t reduce airway inflammation or prevent attacks. Relying on them instead of proven methods like avoidance or immunotherapy can be dangerous. Always consult your doctor before trying alternatives.







Shawna B
14 Nov 2025 at 03:54So just wash bedding in hot water and use a HEPA vacuum? Sounds easy enough. I'll try it this weekend.