When someone is diagnosed with Huntington’s disease, it’s not just a medical label-it’s a life-altering moment for the whole family. There’s no cure. No magic pill. But there is understanding, and with it, a way to take back some control. Huntington’s disease (HD) is a genetic brain disorder that slowly destroys movement, thinking, and emotional stability. It doesn’t come out of nowhere. It’s passed down, gene by gene, with cruel precision. And while the symptoms can be terrifying, especially the uncontrollable jerking movements called chorea, the real turning point comes not from medication, but from care planning.
How Huntington’s Disease Is Inherited
Every child of a parent with Huntington’s has a 50% chance of getting the disease. It doesn’t matter if you’re male or female. It doesn’t matter where you live. If your parent has the mutated gene, you have a coin flip’s chance of inheriting it. This is called autosomal dominant inheritance. One bad copy of the gene is enough to cause the disease. The problem lies in a tiny glitch in the HTT gene on chromosome 4. Normal genes have 10 to 26 repeats of the CAG sequence. When that number climbs to 40 or higher, the body starts making a faulty protein-huntingtin-that slowly kills brain cells. The higher the repeat count, the earlier the symptoms show up. Someone with 55 repeats might start having trouble in their 20s. Someone with 42 might not notice anything until their 40s. What makes it even more unpredictable is something called genetic anticipation. When the gene is passed from father to child, the CAG repeats often grow longer. That means a father who developed symptoms at 50 might have a child who starts showing signs at 25. In fact, 85% of juvenile Huntington’s cases come from the father’s side. Mothers can pass it on too, but the repeats usually stay stable or change only slightly. This isn’t just science. It’s personal. People face agonizing choices: Should I get tested before I have symptoms? If I do, and I’m positive, what do I tell my kids? Many wait until they start noticing movement problems. Others test early to plan their lives-careers, relationships, finances-before things change. Genetic counseling is critical here. In top HD care centers, 95% of at-risk people get counseling before testing. But outside those centers, many never even hear about it.Chorea: The Uncontrollable Dance
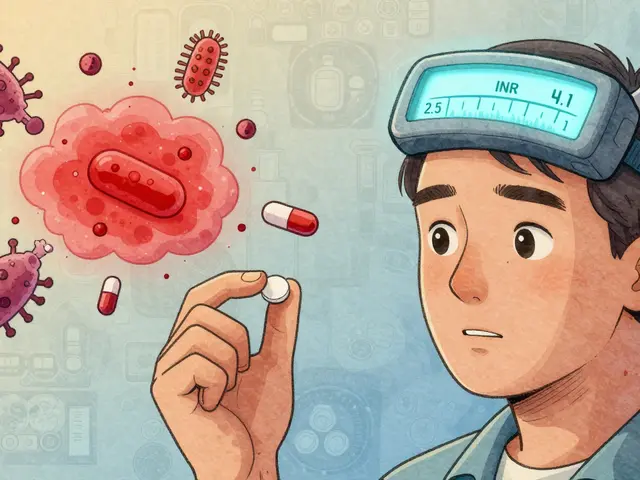
Chorea is the name for the involuntary, dance-like movements that give Huntington’s its early, visible signature. Fingers twitch. Shoulders shrug. Feet shuffle. These aren’t seizures. They’re not meant to be. They’re the brain’s signals going haywire. The movements aren’t constant. They come and go. They get worse when you’re stressed, tired, or trying to focus. And they vanish when you sleep. That’s why many people with early HD are told they’re just “nervous” or “anxious.” It’s easy to miss. Doctors use a tool called the Unified Huntington’s Disease Rating Scale (UHDRS) to measure chorea. A score of 1 means mild, barely noticeable jerks. A score of 4 means constant, wild movements that make sitting, walking, or eating nearly impossible. In advanced stages, chorea doesn’t disappear-it just gets buried under stiffness, slowness, and muscle rigidity. That’s when the real struggle begins. The only FDA-approved drugs for chorea are tetrabenazine (Xenazine) and deutetrabenazine (Austedo). They work by lowering dopamine in the brain, which helps calm the movements. Tetrabenazine can reduce chorea by about 25-30%. But it comes with a heavy cost: depression in 22% of users, drowsiness in 18%. Many patients stop taking it because the side effects feel worse than the chorea itself. Valbenazine (Ingrezza), approved in 2023, offers a slightly better side effect profile. It cuts chorea by about 28%. But neither drug stops the disease. They just manage the symptom. And they’re expensive. Out-of-pocket costs for these drugs can hit $5,000 a year for many families.
Care Planning: The Most Important Treatment
Here’s the truth most people don’t talk about: Medication doesn’t save you. Care planning does. A 2021 study found that people who get coordinated, specialized care live 2.3 years longer than those who don’t. Why? Because their care teams catch problems before they become emergencies. They prevent falls. They stop aspiration pneumonia. They reduce suicide risk by 58%. Care planning isn’t a one-time meeting. It’s a living roadmap that changes as the disease moves through three stages. Early stage (diagnosis to 5 years): This is when you still drive, work, and make decisions. This is the time to get your legal documents in order-living will, healthcare proxy, power of attorney. Only 37% of people in general neurology clinics do this. At HD specialty centers, it’s 82%. That gap is deadly. Mid stage (5 to 15 years): You start needing help with daily tasks. Dressing, bathing, eating. Occupational therapy becomes essential. Speech therapy helps with slurred speech and swallowing problems. By year 10, nearly half of patients need speech therapy. Physical therapy keeps you moving. Aquatic therapy? It’s 35% more effective than land-based exercises for balance. But 68% of patients say they can’t afford it. Late stage (15+ years): You can’t walk. You can’t talk. You need 24/7 care. By year 20, 89% of patients live in residential facilities. The average annual cost? $125,000. Most insurance won’t cover long-term care. Families are left choosing between their savings and their loved one’s dignity. The best care teams include neurologists, psychiatrists, physical therapists, speech therapists, nutritionists, social workers, and genetic counselors-all talking to each other. But here’s the problem: In the U.S., only 38% of neurologists follow the official HD care guidelines. In rural areas, it takes over two years to get a full team together. Urban patients wait about 14 months. That delay costs lives.The Hidden Costs and Emotional Toll
The numbers don’t tell the whole story. One caregiver on the HDSA forum wrote: “The hardest part isn’t the chorea or even knowing I’ll decline-it’s watching my family try to plan for my deterioration while I’m still here.” That’s the emotional weight no drug can touch. Caregivers spend 15+ hours a week managing appointments, insurance, medications, and equipment. Many quit jobs. Many lose savings. Many feel isolated. The Reddit community r/huntington has over 12,000 members, mostly families sharing stories no one else understands. Genetic testing is another emotional minefield. 72% of at-risk people delay testing until symptoms appear. Why? Fear. Guilt. The weight of knowing. Some want to plan. Others don’t want to know. Both choices are valid. But without counseling, neither is informed. And the system is broken. Only 45% of U.S. HD patients have access to a specialized care center. In Europe, it’s 28%. That means most people are left navigating this alone-with a general neurologist who may have never treated a case before.
What’s Next? Hope on the Horizon
There’s real progress. In 2023, Wave Life Sciences reported a drug that reduced the faulty huntingtin protein by 38% in early trials. Roche’s tominersen, after being paused in 2021, is being tested again with safer doses. These aren’t cures yet-but they’re the first real shots at slowing the disease. The Huntington’s Disease Society of America is pushing to expand specialty care centers to cover 85% of U.S. patients by 2025. That’s ambitious. But necessary. Dr. Rachel Andre at Johns Hopkins put it plainly: “Even with successful gene therapies, comprehensive care planning will remain critical for the 40,000+ Americans currently living with HD symptoms.” That’s the truth. We may one day stop Huntington’s. But today, we still need to care for the people living with it. And that means more than pills. It means listening. Planning. Coordinating. Showing up.What You Can Do Now
If you or someone you love has Huntington’s:- Find a certified HD care center. The HDSA lists 53 in the U.S.
- Get genetic counseling-even if you’re not sure about testing.
- Start legal and financial planning now. Don’t wait.
- Connect with others. Join a support group. You’re not alone.
- Ask for physical and speech therapy. Even if insurance says no, ask anyway.
- Document your care preferences. Who speaks for you if you can’t?
- Take breaks. Burnout kills faster than HD.
- Track symptoms with a journal. Small changes matter.
- Know your rights. Medicaid, Medicare, and disability benefits can help.
- Reach out. Other caregivers understand better than anyone.
Is Huntington’s disease inherited from the mother or father?
Huntington’s disease can be inherited from either parent. Each child of an affected parent has a 50% chance of getting the mutated gene, no matter the gender. But when the gene comes from the father, the CAG repeat often expands more, leading to earlier onset-especially in juvenile cases. About 85-90% of childhood-onset Huntington’s is passed down from the father.
Can you get Huntington’s disease if neither parent has it?
It’s extremely rare, but possible. In about 1-3% of cases, a person develops Huntington’s without a known family history. This usually happens when a parent carries an intermediate allele (27-35 CAG repeats), which doesn’t cause symptoms but can expand into the disease-causing range (40+) when passed on. Genetic testing can clarify this.
Does chorea get worse over time in Huntington’s?
Yes, chorea typically worsens in the early and middle stages. But in late-stage HD, chorea often decreases as muscles become stiff and rigid (dystonia and bradykinesia take over). This doesn’t mean improvement-it means the disease has moved deeper into the brain, affecting movement control differently. The overall loss of motor function continues.
Are there any new treatments for Huntington’s disease in 2025?
As of 2025, there are still no cures, but several promising drugs are in late-stage trials. Wave Life Sciences’ SELECT-HD trial showed a 38% reduction in the faulty huntingtin protein. Roche’s tominersen is being tested again with adjusted dosing after being paused in 2021. Valbenazine (Ingrezza) is now approved as a second chorea treatment. These are not cures, but they represent the first real progress in slowing the disease’s progression.
How long do people live after being diagnosed with Huntington’s?
On average, people live 15 to 20 years after symptoms begin. Those with juvenile-onset HD (before age 20) usually live 10 to 15 years after diagnosis. Death often results from complications like pneumonia, heart failure, or injuries from falls. People who receive coordinated, specialized care live an average of 2.3 years longer than those who don’t.
Can physical therapy help someone with Huntington’s disease?
Yes, physical therapy is one of the most effective non-drug tools. It helps maintain mobility, reduce fall risk, and improve balance. Aquatic therapy-exercises in water-is 35% more effective than land-based therapy for balance in HD patients. Many patients report improved confidence and independence with regular sessions, even in later stages.
What’s the best way to plan for long-term care in Huntington’s?
Start early. Work with a care team that includes a social worker and financial planner. Document your wishes in a living will and healthcare proxy. Explore Medicaid and long-term care insurance options. Consider residential care facilities that specialize in neurodegenerative diseases. Most families wait too long-by the time they need help, the system is overwhelmed. Planning before crisis hits saves lives.






Souhardya Paul
16 Dec 2025 at 10:55Just wanted to say this post nailed it. I’ve been watching my dad go through HD for 8 years now, and the part about care planning being the real treatment? That’s the only thing that kept us from falling apart.
Getting that living will done before he lost speech? Life-saving. No one talks about how much stress that paperwork relieves until you’re in it.
Also, aquatic therapy saved his balance. We did it twice a week. He’d come out smiling, even when he couldn’t walk straight. Worth every penny.
Thanks for writing this. Someone needed to say it out loud.