Medication Fat Calculator
Optimal Fat Amount Calculator
Find out how much fat you need to take with lipid-based medications for best absorption.
Results
Select a medication and enter fat amount to see results
Important: High-fiber foods like bran cereal can block absorption. Avoid these with lipid-based medications.
Why Some Pills Work Better With a Fatty Meal
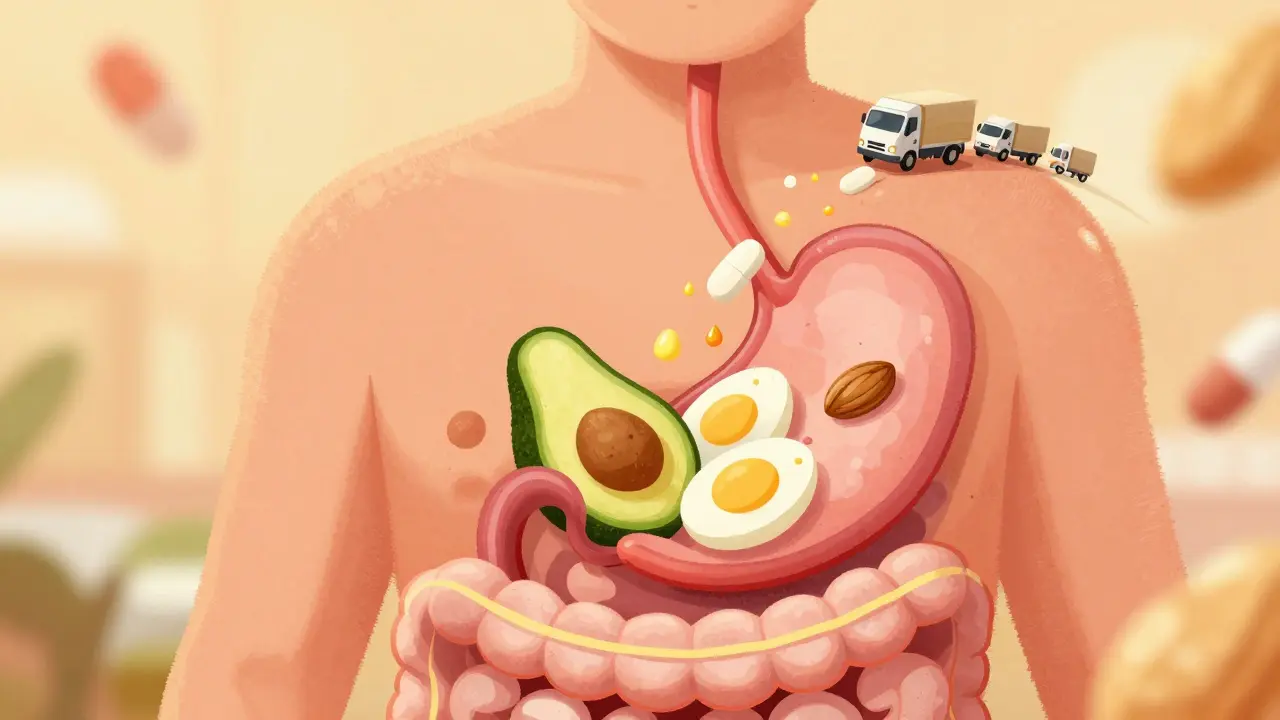
Have you ever been told to take your medication with food-especially something oily like avocado, nuts, or eggs? It’s not just to avoid an upset stomach. For certain drugs, fat isn’t just helpful-it’s essential. Without it, the medicine might not work at all.
Up to 70% of new drugs being developed today are poorly soluble in water. That means they don’t dissolve well in your gut, so your body can’t absorb them properly. This is where fatty foods and lipid-based medications come in. They don’t just help the drug dissolve-they actively make your body absorb more of it.
The Science Behind the Food Effect
The connection between fat and drug absorption is called the "food effect." It’s not a myth. It’s been studied for decades. When you eat fat, your body releases bile and digestive enzymes. These break down the fat into tiny droplets that can trap drug molecules, keeping them suspended so they’re ready to be absorbed.
Researchers like Christopher Porter at Monash University showed in the early 2000s that these fat breakdown products, combined with bile salts, form structures called micelles and mixed micelles. These act like tiny delivery trucks, carrying drugs through the gut lining and into your bloodstream. Without fat, those drugs just sit there, undissolved and useless.
Studies show lipid-based formulations can boost absorption by 20% to over 300%. For example, cyclosporine (used after organ transplants) sees a 20-30% increase in absorption when taken with fat. Fenofibrate (for cholesterol) gets 31% more into the bloodstream compared to older versions that didn’t use fat-based carriers.
What Makes a Fat "Good" for Medication?
Not all fats are created equal when it comes to helping drugs. Medium-chain triglycerides (MCTs), found in coconut oil and some pharmaceutical oils, work better than long-chain fats like butter or olive oil.
Why? MCTs digest faster. They break down in 15-30 minutes in the small intestine. Long-chain fats take over an hour. That speed matters because the drug needs to stay dissolved while the gut is most active. If the fat takes too long to break down, the drug might clump up and get excreted.
Pharmaceutical companies use specific oils like Capmul MCM, which is made of MCTs, in their formulations. These are mixed with surfactants (like Tween 80) and cosolvents (like Transcutol HP) to create self-emulsifying systems. When swallowed, they turn into a fine milky liquid-no chewing needed. The droplets are only 100-300 nanometers wide, which lets them slip through the gut lining easily.
Medications That Rely on Fat
Some of the most important drugs in modern medicine need fat to work:
- Itraconazole (Sporanox®): An antifungal. The liquid version with fat absorbs 2.8 times better than the capsule, even on an empty stomach.
- Cyclosporine (Neoral®): Used for transplant patients. The lipid version means you don’t have to time meals perfectly anymore.
- Fenofibrate (Tricor®): Lowers triglycerides. Patients report fewer stomach issues and can take it once a day instead of three times.
- Vybar (fenofibric acid): The newest lipid-based version, approved in 2022, boosts absorption by 45% and removes food effects entirely.
These aren’t niche drugs. They’re used by millions. Without lipid-based delivery, many patients would need higher doses, more frequent pills, or even injections.

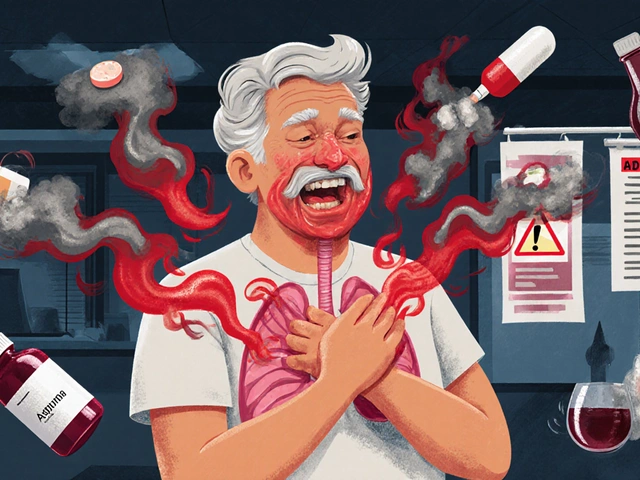
When Fat Doesn’t Help-Or Hurts
Not every drug benefits from fat. Drugs that dissolve easily in water (BCS Class I) don’t need it. In fact, fat can slow them down by delaying stomach emptying.
Bisphosphonates like alendronate (Fosamax®), used for osteoporosis, need an empty stomach and plain water. Fat can interfere with their absorption. Same goes for antibiotics like tetracycline-fat reduces how much gets into the blood.
Patients with digestive disorders (Crohn’s, cystic fibrosis, gallbladder removal) may not produce enough bile. That means lipid-based drugs might not work as well for them. Doctors have to adjust doses or switch formulations in these cases.
Real Patient Experiences
People who take these medications regularly notice the difference.
One Reddit user, u/TransplantSurvivor, wrote: "Switching from Sandimmune to Neoral eliminated my need to plan meals around my pills. I could eat normally again." Another, u/CholesterolWarrior, said: "Tricor doesn’t give me the stomach cramps the old version did. I actually take it now without thinking about it."
But there’s a downside: cost. Sporanox oral solution costs about $1,200 for a month’s supply. The generic capsule version? Around $300. Many patients can’t afford the lipid version, even if it’s more effective. Insurance doesn’t always cover it unless you’ve tried the cheaper option first.
Why These Formulations Are Hard to Make
Creating a lipid-based drug isn’t like making a regular pill. It’s like cooking a precise recipe with chemicals.
Formulators test 80-100 different fat-surfactant combinations for each drug. They build phase diagrams to see how the mixture behaves under gut conditions. Then they run in vitro lipolysis tests-simulating digestion in a lab-to predict how the drug will behave in real people.
This process takes 18-24 months, compared to 12-15 months for standard tablets. It’s expensive. Manufacturing costs are 25-35% higher. That’s why lipid-based drugs are often branded and not available as generics.
Only big pharma companies with deep pockets and specialized labs can do this well. Smaller manufacturers often lack the data or tools to optimize these formulations.

The Future: Smart Lipid Capsules
The next wave of lipid-based delivery is getting smarter.
MIT researchers developed a prototype capsule in 2023 that senses pH and enzyme levels in the gut. It adjusts how fast it releases the drug based on what’s happening in real time. That means it could work equally well whether you eat a salad or a burger.
Matinas BioPharma’s LNC technology already showed 92% bioavailability for amphotericin B in trials-compared to just 30% with older forms. That’s a game-changer for treating serious fungal infections.
Regulators like the FDA and EMA now require detailed studies on how these drugs interact with food. That means future formulations will be more predictable, safer, and tailored to real-world eating habits.
What You Should Do
If you’re on a medication that might be affected by food:
- Check the label. Does it say "take with food" or "take on an empty stomach"?
- If it says "with food," use a meal with at least 15-20 grams of fat. A tablespoon of olive oil, a handful of almonds, or a slice of cheese qualifies.
- Don’t assume all fats are equal. Avoid high-fiber meals (like bran cereal) with lipid drugs-they can bind to the drug and block absorption.
- If you have digestive issues, talk to your pharmacist. You might need a different formulation.
- If cost is a barrier, ask about patient assistance programs. Some manufacturers offer discounts or free samples.
For doctors and pharmacists: Know which drugs are lipid-dependent. Don’t substitute them with generic versions unless you’re sure the alternative has the same delivery system.
Why This Matters
Lipid-based delivery isn’t just a clever trick. It’s solving a real problem: too many drugs don’t work because they won’t dissolve. Fat isn’t the enemy-it’s the ally we’ve learned to harness.
As more drugs enter the pipeline with poor solubility, this technology will become more common. By 2028, the market for these formulations is expected to hit $9.2 billion. That’s because the science works.
For patients, it means fewer pills, fewer side effects, and better outcomes. For the system, it means smarter, more effective treatments that actually get absorbed-no magic, just biology.







Write a comment