Warfarin-Antibiotic Safety Checker
Check Antibiotic Safety with Warfarin
Select an antibiotic to see its risk level with warfarin and recommended monitoring steps
When you're on warfarin, even a simple antibiotic can throw your blood thinning out of balance - and that’s not just a minor concern. It can mean the difference between a quick recovery and a trip to the ER with internal bleeding. This isn’t theoretical. Every year, thousands of people on warfarin end up in hospital because their INR spiked after starting an antibiotic. And most of the time, it was avoidable.
Why Antibiotics Change Your INR
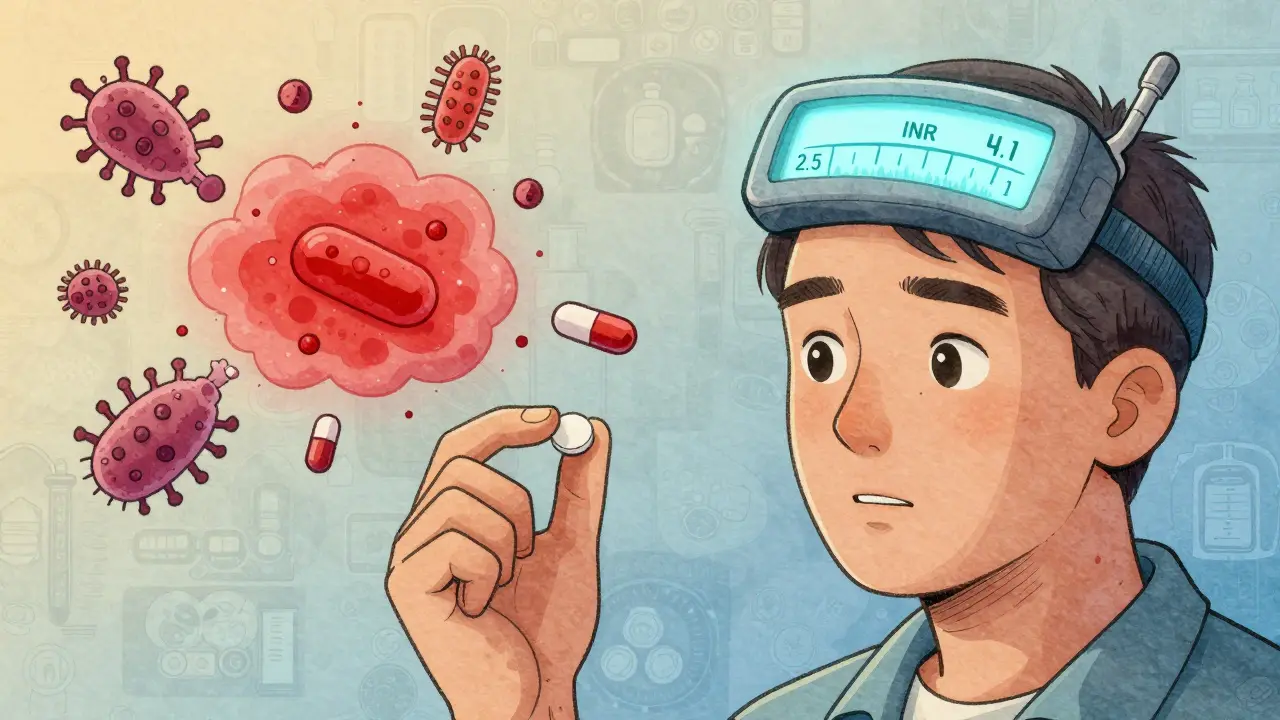
Warfarin works by blocking vitamin K, which your body needs to make clotting factors. But your gut bacteria also make vitamin K - about 10-15% of what you need. When antibiotics wipe out those bacteria, your vitamin K drops, and your blood thins even more. That’s one reason your INR climbs. The other reason? Your liver. Warfarin is broken down by enzymes called CYP450, especially CYP2C9. Some antibiotics block these enzymes, so warfarin builds up in your blood. That’s like turning up the dose without changing the pill. Ciprofloxacin, erythromycin, and Bactrim are big culprits. They can push your INR from 2.5 to 4.1 in less than a week. Not all antibiotics do this. Nitrofurantoin and fosfomycin? Safe. Azithromycin? Low risk. But if your doctor prescribes ciprofloxacin for a UTI or amoxicillin/clavulanate for a sinus infection, you’re in the danger zone.Which Antibiotics Are Most Dangerous?
Here’s what actually happens in real patients, based on data from over 30,000 people:- Ciprofloxacin - INR jumps 1.5-2 units on average. Bleeding risk up 2.1 times.
- Bactrim (sulfamethoxazole/trimethoprim) - INR rises by 1.8 units in 5 days. One of the top offenders.
- Amoxicillin/clavulanate - No CYP effect, but still raises INR by 1.2 units. Gut flora disruption.
- Erythromycin - Strong CYP3A4 blocker. Bleeding risk 2.3 times higher.
- Cefotetan - A cephalosporin with a risky side chain. INR spikes up to 2.2 units.
- Rifampin - The opposite problem. Makes warfarin break down faster. INR can crash below 1.5. Risk of clotting.
- Azithromycin, ceftriaxone, nitrofurantoin - Minimal to no effect. Often safe choices.
It’s not about the class name - it’s about the specific drug. Even within penicillins or cephalosporins, some are risky, others aren’t. Your doctor might not know the difference. You need to.
When the INR Spike Hits - And How to Spot It
The biggest danger? The spike doesn’t come when you start the antibiotic. It comes later. CYP enzyme effects? They hit in 2-3 days. Gut flora effects? They take 5-7 days. That’s why people feel fine at first, then suddenly get dizzy, bruise easily, or notice blood in their urine - and they blame it on “getting older.” Bleeding signs you can’t ignore:- Unexplained bruising - especially large, dark patches
- Bleeding gums when brushing teeth
- Nosebleeds that won’t stop
- Red or black stools
- Dark, coffee-ground vomit
- Prolonged bleeding from cuts
- Headaches, confusion, or vision changes (could mean brain bleed)
INR above 4.0? That’s a red flag. Your risk of major bleeding jumps 4 to 8 times. Above 5.0? Emergency territory.

What You Should Do - Step by Step
If you’re on warfarin and your doctor prescribes an antibiotic:- Ask: “Is this antibiotic safe with warfarin?” Don’t assume it’s fine. Bring this list with you.
- Get your INR checked within 72 hours of starting the antibiotic - even if you feel fine.
- Check again 3-4 days later - gut effects take time.
- Check again 3 days after stopping - vitamin K levels rebuild slowly. INR can still climb after the antibiotic is gone.
- Don’t change your warfarin dose yourself. Your anticoagulation clinic will adjust it based on your INR trend, not a single number.
- If you’re on ciprofloxacin, Bactrim, or erythromycin, your dose may need to be lowered by 20-30% upfront. Don’t wait for a spike.
- If you’re on rifampin, your warfarin dose will likely need to go up - sometimes by 50% or more.
Some clinics now use pharmacist-led management. Studies show this cuts bleeding by 37%. Ask if your provider offers this. If not, push for it.
What to Do If You’re Already Bleeding
If you notice any bleeding symptoms:- Call your anticoagulation clinic or GP immediately.
- Do NOT stop warfarin on your own - that can cause clots.
- Go to the ER if you have: chest pain, trouble breathing, severe headache, vomiting blood, or sudden weakness.
- Bring your warfarin bottle and a list of all recent medications - including OTC drugs and supplements.
Emergency treatment may include vitamin K (oral or IV), fresh frozen plasma, or even prothrombin complex concentrate. But prevention beats treatment every time.
What’s New in 2026
We’re moving beyond one-size-fits-all rules. Genetic testing for CYP2C9 variants (like *2 and *3) is now available through some NHS and private labs. People with these variants see INR spikes 2.4 times higher when taking antibiotics. If you’ve had multiple unexplained INR changes, ask about testing. New antibiotics like tedizolid? Safe. No INR effect. If you’re on long-term antibiotics (like for bone infections), ask if a safer option exists. Electronic alerts in EHRs help - but only if they’re smart. A 2019 study found simple pop-up warnings reduced events by just 7%. But when paired with clinical decision support - like automatic INR order suggestions - the drop was 22%.Bottom Line: Stay in Control
Antibiotics and warfarin don’t have to be a dangerous combo. But you can’t rely on your doctor to catch every interaction. You need to be your own advocate. Remember: Not all antibiotics are equal. Some are safe. Some are risky. Some are deadly when paired with warfarin.- Check your INR before, during, and after antibiotics.
- Know which ones to avoid.
- Watch for bleeding - even small signs.
- Ask for pharmacist support.
- Don’t wait for symptoms to act.
Every year, 42% of warfarin-related ER visits involve antibiotics. Most of them are preventable. You don’t need to be another statistic.
Can I take amoxicillin while on warfarin?
Amoxicillin alone is usually safe, but amoxicillin/clavulanate (Augmentin) can raise your INR by about 1.2 units on average. This isn’t due to liver enzyme changes - it’s because clavulanate disrupts gut bacteria that make vitamin K. Get your INR checked 5-7 days after starting it. Don’t assume it’s harmless just because it’s a common antibiotic.
How long does it take for warfarin to return to normal after an antibiotic?
It depends on the antibiotic. If it affected liver enzymes (like ciprofloxacin), your INR should drop back to normal within 3-5 days after stopping. But if it wiped out gut bacteria (like amoxicillin/clavulanate or cefotetan), it can take 7-14 days for vitamin K levels to rebuild. That’s why you need to keep checking your INR for at least a week after finishing the antibiotic - even if you feel fine.
Is azithromycin safe with warfarin?
Yes, azithromycin is one of the safest antibiotics to take with warfarin. It doesn’t significantly block CYP enzymes or disrupt gut flora. Studies show only a 1.2-fold increase in bleeding risk - which is not statistically significant. If you need a macrolide, azithromycin is your best bet. Always confirm with your clinic, but you’re far less likely to have a problem than with erythromycin or ciprofloxacin.
Should I take vitamin K supplements to prevent INR spikes?
No. Taking extra vitamin K without medical supervision can make your warfarin ineffective and increase your risk of clots. The problem isn’t low vitamin K intake - it’s your gut bacteria not making enough. Eating leafy greens is fine, but don’t suddenly start taking supplements. Your INR should be managed by your anticoagulation team with precise warfarin adjustments, not by diet changes.
Why do some doctors say antibiotics don’t affect warfarin?
Some older guidelines downplayed the risk, especially for antibiotics like amoxicillin. But recent data from 2023-2024 confirms that even “low-risk” antibiotics can cause dangerous INR spikes. The 2024 systematic review in Expert Opinion on Drug Metabolism & Toxicology found cephalosporins increase bleeding risk by 1.9-fold. Many doctors haven’t updated their knowledge. Don’t rely on outdated advice. Ask for current guidelines or ask to speak with a pharmacist who specializes in anticoagulation.
What if I need an antibiotic but can’t get my INR checked?
If you’re unable to get your INR tested within 72 hours of starting an antibiotic, delay the antibiotic if possible. For non-urgent infections, wait until you can monitor your INR. If it’s urgent (like sepsis), go to the ER and ask for an immediate INR test. Do not start the antibiotic without knowing your baseline INR. If you’re on a high-risk antibiotic like ciprofloxacin or Bactrim and can’t get tested, ask your doctor about switching to a safer alternative like azithromycin or nitrofurantoin.








Solomon Ahonsi
2 Feb 2026 at 00:32This post is basically a 2000-word PSA for people who can’t read a drug label. I’ve been on warfarin for 8 years and never once had my doctor mention any of this. Guess what? I’m still alive. But now I’m supposed to memorize which antibiotics are ‘safe’ like it’s a damn trivia game? Ridiculous.