Anticoagulant Bleeding Risk Calculator
Assess Your Bleeding Risk
Your Bleeding Risk Assessment
When someone takes a blood thinner, they’re trading one risk for another. The goal is to stop dangerous clots from forming-like those that cause strokes or pulmonary embolisms-but every dose also raises the chance of serious bleeding. This isn’t theoretical. About 1-3% of people on anticoagulants experience a major bleed each year. For older adults or those with kidney problems, that risk jumps even higher. The key isn’t avoiding blood thinners-it’s managing them smartly so the benefits far outweigh the dangers.
How Anticoagulants Work-and Why They Bleed
Anticoagulants don’t actually "thin" the blood. They interrupt the clotting process. Warfarin, the oldest of these drugs, blocks vitamin K, which your liver needs to make clotting factors. Newer drugs, called DOACs (direct oral anticoagulants), target specific proteins in the clotting cascade: dabigatran blocks thrombin, while apixaban, rivaroxaban, and edoxaban block factor Xa. Heparins work by boosting antithrombin, a natural brake on clotting. All of them slow clot formation. That’s good when you have atrial fibrillation or a mechanical heart valve. But if you cut your finger, hit your head, or have an internal bleed, your body can’t stop the bleeding as quickly. That’s why hemorrhage prevention isn’t about avoiding anticoagulants-it’s about reducing the chance that bleeding becomes life-threatening.Who’s at Highest Risk for Bleeding?
Not everyone on blood thinners is equally likely to bleed. Some people face much higher risks:- People over 75: They’re two to three times more likely to bleed than younger adults.
- Those with kidney problems: If your creatinine clearance (CrCl) is below 50 mL/min, your bleeding risk doubles. For DOACs like rivaroxaban and apixaban, this means dose adjustments are mandatory.
- Patients on multiple blood-thinning drugs: Taking aspirin, clopidogrel, or NSAIDs like ibuprofen with a blood thinner can raise major bleeding risk by 50-70%.
- People with uncontrolled high blood pressure: High pressure bursts small vessels-anticoagulants make those bursts harder to stop.
- Those with liver disease or history of GI bleeding: The liver makes clotting factors. If it’s damaged, your body’s backup system is already weak.
One study found that patients with CrCl below 30 mL/min on apixaban had a 40% higher bleeding rate than those with normal kidney function-even when doses were reduced. Renal function isn’t just a number-it’s a red flag.
Warfarin vs. DOACs: Which Is Safer?
For years, warfarin was the only option. It’s cheap-about $4 a month-but it’s tricky to use. You need regular blood tests (INR), and your diet, alcohol, and other meds can throw your dose off. Keeping your INR between 2.0 and 3.0 (or 2.5-3.5 for mechanical mitral valves) is critical. If your time in therapeutic range (TTR) drops below 60%, your bleeding risk rises sharply. DOACs changed the game. They don’t need routine blood tests. Doses are fixed. And overall, they cause 19-20% fewer major bleeds than warfarin. Apixaban stands out: in the ARISTOTLE trial, it cut major bleeding by 31% compared to warfarin. But DOACs aren’t perfect. They’re expensive-apixaban can cost $550 a month without insurance. And while they’re safer for most people, they’re worse for some:- Patients with mechanical heart valves (especially mitral): DOACs increase clot risk here. Warfarin is still the standard.
- People with antiphospholipid syndrome: DOACs have higher rates of recurrent clots in this group.
For most others-especially those with atrial fibrillation or a history of deep vein thrombosis-DOACs are the better choice today.
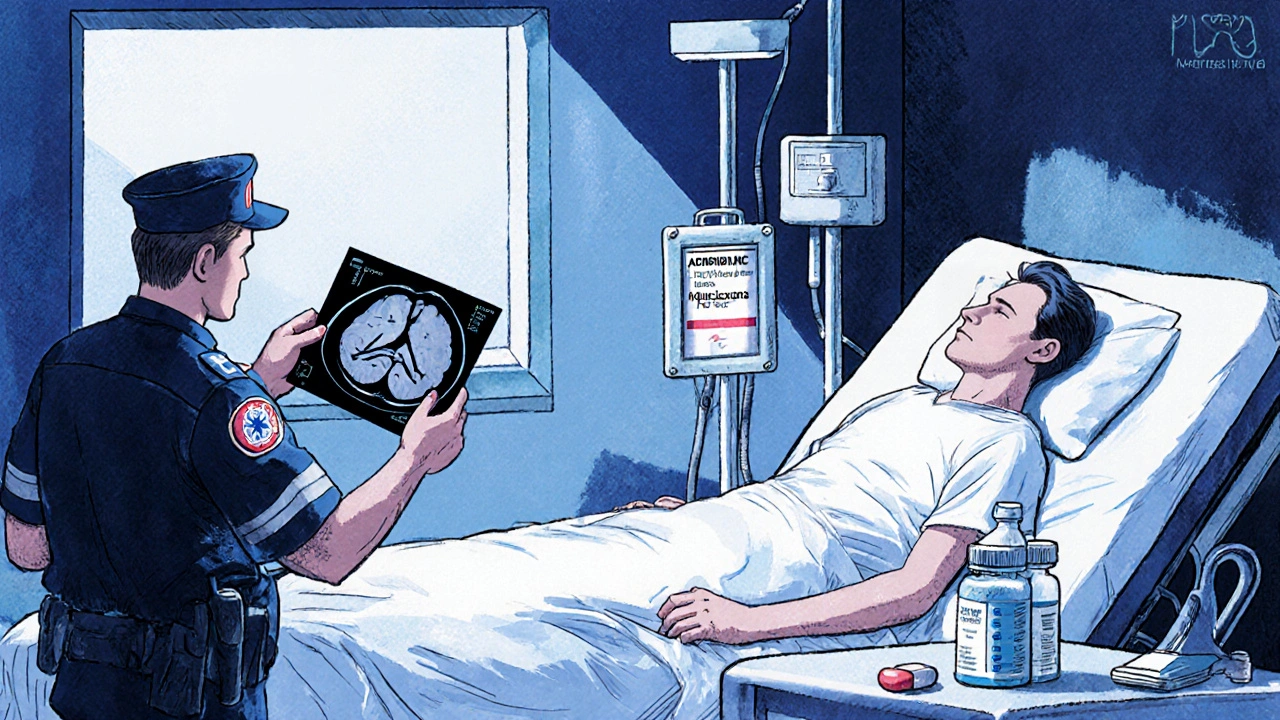
Reversing Anticoagulants in an Emergency
If a patient on a blood thinner has a brain bleed, a major trauma, or uncontrolled GI bleeding, you need to reverse the drug fast. Time matters. Minutes count. Here’s what works:- Warfarin: Use four-factor prothrombin complex concentrate (4f-PCC) at 25-50 units/kg. It fixes INR in 15 minutes. Vitamin K (5-10 mg IV) helps too, but it takes hours to work-so use it as backup, not first-line.
- Dabigatran: Idarucizumab (Praxbind) is the specific antidote. One 5g IV dose reverses its effect within minutes.
- Rivaroxaban, apixaban, edoxaban: Andexanet alfa (Andexxa) is the reversal agent. It’s effective, but it costs about $13,000 per dose-and many hospitals don’t keep it on hand.
- Heparin: Protamine sulfate reverses unfractionated heparin well (60-100% neutralization). It’s much less effective for low-molecular-weight heparins like enoxaparin.
Many ERs still don’t have reversal agents stocked. That’s why prevention matters more than reversal. If you’re managing someone on a DOAC, know what’s available at your hospital. If you’re a patient, ask your doctor: "What if I bleed? What’s the plan?"
Practical Steps to Prevent Bleeding
You can’t eliminate bleeding risk-but you can cut it in half with smart habits:- Check kidney function every 3-6 months. If you’re on a DOAC and your CrCl drops below 30 mL/min, your dose may need adjusting-or switching.
- Avoid NSAIDs and aspirin. Use acetaminophen for pain instead. Even low-dose aspirin increases bleeding risk when combined with anticoagulants.
- Use a pill organizer. Dosing errors are common in older adults. Taking two doses by accident is a leading cause of emergency visits.
- Wear a medical alert bracelet. It tells first responders you’re on a blood thinner-critical if you’re unconscious after a fall.
- Don’t stop your medication without talking to your doctor. Stopping warfarin or a DOAC suddenly can trigger a clot within days.
- Be cautious with alcohol. Heavy drinking throws off warfarin metabolism and increases bleeding risk.
One study found that patients who used pill organizers and had monthly kidney checks reduced their bleeding risk by 45% compared to those who didn’t.
What About Bleeding Disorders?
This isn’t just about anticoagulants. Some people have inherited bleeding disorders-like hemophilia or von Willebrand disease. They may need anticoagulants for other reasons (like atrial fibrillation) but are at extreme risk of bleeding. In these cases, doctors may use desmopressin (DDAVP), which boosts von Willebrand factor and factor VIII. A 2021 trial showed it significantly reduced blood loss in women with bleeding disorders undergoing procedures. It’s not a cure-but it’s a tool. For people with severe hemophilia, factor replacement therapy may be needed alongside anticoagulation. This requires close coordination between hematologists and cardiologists.
When to Restart Anticoagulation After a Bleed
Many patients stop their blood thinner after a bleed-and never restart. That’s often a mistake. The American College of Cardiology says: restart as soon as it’s safe. For most people, that’s within days to a week. The risk of a clot returning is higher than the risk of another bleed. Here’s the rule of thumb:- If your stroke risk is low (e.g., CHA₂DS₂-VASc score under 2-3, or a provoked blood clot that happened more than 3 months ago), stopping may be okay.
- If your stroke or clot risk is high (e.g., permanent atrial fibrillation, mechanical valve, unprovoked DVT), restart anticoagulation. The data shows survival improves.
Delaying restart increases the chance of a fatal clot. Waiting too long to restart is just as dangerous as bleeding in the first place.
The Future: Better Tools, Fewer Bleeds
Researchers are working on solutions:- Ciraparantag: A universal reversal agent in trials. If it works, it could reverse all DOACs and heparins with one shot.
- Point-of-care DOAC tests: Like an INR machine, but for apixaban or rivaroxaban. These could let doctors see exactly how much drug is in the blood-helping decide if reversal is needed.
- AI risk predictors: New models are being trained to predict bleeding risk based on age, kidney function, meds, and even genetics.
One modeling study estimated that if all DOAC users had access to point-of-care testing, major bleeding events could drop by 15-20%.
The bottom line? Anticoagulants save lives. But they demand respect. The goal isn’t to avoid them-it’s to use them with precision. Know your risk. Know your drug. Know your reversal plan. And never stop without talking to your doctor.
Can I take ibuprofen if I’m on a blood thinner?
No. Ibuprofen and other NSAIDs like naproxen significantly increase bleeding risk when combined with anticoagulants. Use acetaminophen (Tylenol) instead for pain or fever. Even low-dose aspirin raises bleeding risk by 50-70% when taken with blood thinners.
Do I need blood tests if I’m on apixaban or rivaroxaban?
Routine blood tests like INR aren’t needed for DOACs like apixaban or rivaroxaban. But your kidney function (CrCl) must be checked every 3-6 months. If you’re over 75, have diabetes, or have kidney disease, your doctor may check it more often. Dosing depends on kidney health-so skipping these tests can be dangerous.
Is warfarin still used today?
Yes. While DOACs are now the first choice for most people, warfarin is still the standard for mechanical heart valves (especially mitral valves) and antiphospholipid syndrome. DOACs have higher clotting rates in these conditions. Warfarin is also used when cost is a barrier-since it’s under $5 a month, unlike DOACs that cost hundreds.
What should I do if I fall and hit my head while on a blood thinner?
Even if you feel fine, go to the ER. A brain bleed can develop slowly. Don’t wait for symptoms like headache, dizziness, or confusion. Tell the staff you’re on a blood thinner and name the drug. Bring your medication list. Early imaging (like a CT scan) can catch bleeding before it becomes life-threatening.
Can I drink alcohol while on anticoagulants?
Moderate alcohol is usually okay-one drink a day for women, two for men. But heavy drinking (more than 3 drinks at once) interferes with how warfarin works and can raise bleeding risk. With DOACs, alcohol doesn’t interact directly, but binge drinking increases fall risk-and falls with anticoagulants can mean serious injury.
What happens if I miss a dose of my blood thinner?
If you miss a dose of a DOAC (like apixaban), take it as soon as you remember-if it’s within 6 hours of your usual time. If it’s been longer, skip the missed dose and take your next one at the regular time. Never double up. For warfarin, skip the missed dose and resume your schedule the next day. Never take two doses to make up for one. Missing doses increases clot risk; doubling doses increases bleeding risk.
Are there natural alternatives to blood thinners?
No. Supplements like garlic, ginger, fish oil, or vitamin E don’t replace anticoagulants. They may slightly increase bleeding risk on their own, but they don’t prevent strokes or clots effectively. Relying on them instead of prescribed medication can be deadly. Always tell your doctor if you’re taking supplements-they can interact dangerously with blood thinners.
How do I know if I’m bleeding internally?
Signs include unusual bruising, blood in urine or stool (dark or tarry), vomiting blood, severe headaches, dizziness, weakness, or sudden pain in the abdomen, back, or joints. If you feel suddenly weak or faint, or if your skin looks pale or clammy, get help immediately. Internal bleeding can be silent until it’s serious.
Next Steps: What to Do Now
If you’re on a blood thinner:- Ask your doctor: "What’s my bleeding risk?" and "What’s the plan if I bleed?"
- Get your kidney function checked-don’t wait for symptoms.
- Stop taking NSAIDs or aspirin unless your doctor says it’s safe.
- Wear a medical alert bracelet.
- Keep a current list of all your meds-including supplements-and carry it with you.
If you’re a caregiver or family member:
- Help with pill organization.
- Watch for signs of bleeding.
- Know which hospital has reversal agents on hand.
Anticoagulants aren’t dangerous because they’re bad drugs. They’re dangerous because they’re powerful-and used without enough attention. The best way to prevent hemorrhage isn’t to stop the medicine. It’s to use it with knowledge, care, and a clear plan.




Neoma Geoghegan
23 Nov 2025 at 22:47DOACs are game changers but kidney checks are non-negotiable. Skip the labs and you’re playing Russian roulette with internal bleeding.
Get CrCl checked every 3 months or don’t bother taking it.