DOAC Switch Safety Calculator
Input Your Medical Data
Switching Recommendations
Please enter your data to see recommendations
This tool provides general guidance only. Always consult your healthcare provider before switching medications.
Switching from warfarin to a direct oral anticoagulant (DOAC) can simplify your life-no more weekly blood tests, fewer food restrictions, and less risk of dangerous bleeding. But if done wrong, it can also put you at serious risk of stroke or internal bleeding. This isn’t a simple swap. It’s a medical transition that needs precision, timing, and clear understanding. If you’re considering this change, here’s what actually matters.
Why Switch at All?
Warfarin has been the go-to blood thinner for over 70 years. But it’s finicky. You need regular INR blood tests-often every 1 to 4 weeks-to make sure your dose is right. Too low, and you risk a clot. Too high, and you could bleed internally. Even small changes in diet, other meds, or illness can throw your INR off. That’s why millions of people are switching to DOACs: dabigatran, rivaroxaban, apixaban, and edoxaban. DOACs don’t need routine blood monitoring. They work more predictably. Studies show they’re just as good at preventing strokes in atrial fibrillation, and they cut the risk of brain bleeds by nearly 30% compared to warfarin. They also interact with fewer drugs and foods. For most people, that’s a huge win.But Not Everyone Can Switch
This isn’t a one-size-fits-all move. Some people should never switch. If you have a mechanical heart valve, DOACs won’t work for you. They’re not approved for this use, and switching could lead to a life-threatening clot. Same goes if you’re pregnant or breastfeeding-warfarin is still the safer choice here. Kidney function matters too. DOACs are cleared through the kidneys. If your creatinine clearance (CrCl) is below 15-30 mL/min, depending on the drug, you might not be a candidate. For example, edoxaban and dabigatran are usually avoided if CrCl is under 30. Apixaban is the most forgiving in mild-to-moderate kidney disease, but even then, dose adjustments are needed. Liver disease is another red flag. If you have severe liver impairment (Child-Pugh Class C), your body can’t process these drugs properly. That increases bleeding risk. And if you weigh less than 60 kg or more than 150 kg, you were barely studied in trials. Your doctor needs to be extra careful.The Critical Timing Rule: INR Is Your Guide
This is where most mistakes happen. You can’t just stop warfarin and start a DOAC the next day. You need to know your INR level at the exact moment you switch. Here’s what the guidelines say:- If your INR is ≤2.0: Start the DOAC right away.
- If your INR is 2.0-2.5: Start the DOAC the same day or the next day.
- If your INR is 2.5-3.0: Wait 1 to 3 days. Recheck your INR.
- If your INR is ≥3.0: Delay the switch. Recheck in 3 to 5 days.
- Rivaroxaban: Safe to start when INR ≤3.0
- Edoxaban: Only start when INR ≤2.5
- Apixaban and dabigatran: Require INR ≤2.0
Side Effects You Might Not Expect
DOACs are safer overall, but they’re not side-effect-free. The most common issue during the switch? Gastrointestinal bleeding. It’s rare, but it happens more often right after switching, especially with dabigatran. That’s because of the overlap in drug effects. Also, DOACs can temporarily raise your INR. Don’t panic if your next blood test shows a higher number. That doesn’t mean you’re over-anticoagulated. DOACs interfere with the test itself. Your doctor needs to know you’re on a DOAC so they don’t misread the results. Another hidden risk: forgetting to take your pill. Unlike warfarin, where missing a dose gives you a buffer, DOACs leave your system in 12 to 24 hours. Miss one dose, and your protection drops fast. That’s especially dangerous if you have atrial fibrillation-you could have a stroke within hours.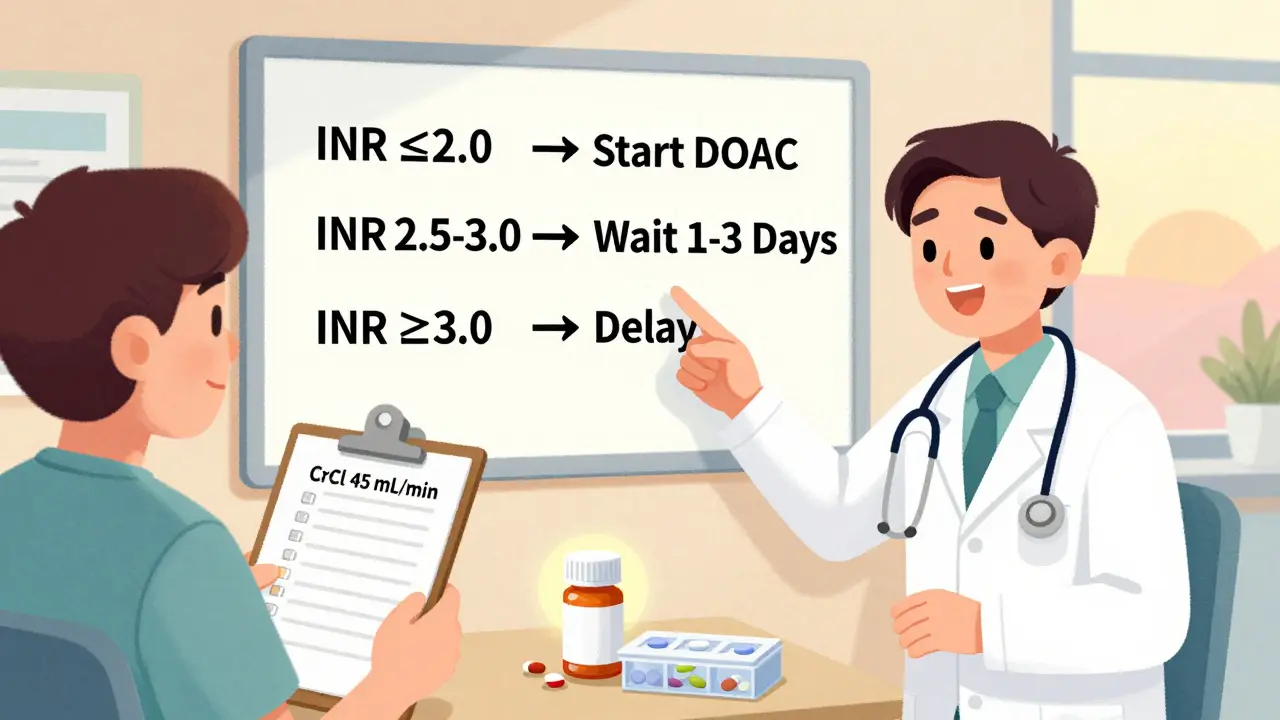
Dabigatran Has Special Rules
Dabigatran is moisture-sensitive. If you put it in a pill organizer, it can lose potency. You must keep it in its original bottle. Other DOACs like apixaban and rivaroxaban are fine in dosette boxes. But dabigatran? Not unless you’re using a special humidity-proof container. Also, if you need surgery or a dental procedure, timing matters. For low-risk procedures, hold dabigatran for 24 to 36 hours if your kidneys are normal. If your CrCl is 45 mL/min or lower, hold it for 96 to 108 hours. Your doctor should give you a written plan.What Your Doctor Must Check Before Switching
A good transition isn’t just about the switch day. It starts weeks before. Your doctor should review:- Your last INR (within the past month)
- Your recent kidney function (CrCl from Cockcroft-Gault formula)
- Your liver enzymes and blood counts (FBC, LFTs)
- All your other medications (especially NSAIDs, SSRIs, antibiotics)
- Your weight and age
Patient Education Is Non-Negotiable
You’re not just a patient-you’re a partner in this process. You need to know:- Exactly when to stop warfarin and start the DOAC
- What to do if you miss a dose
- Which symptoms mean trouble (dark urine, severe headache, vomiting blood, unexplained bruising)
- That you still need to tell every doctor, dentist, and pharmacist you’re on a blood thinner

Cost and Access Still Matter
In the U.S., DOACs cost $500 to $700 a month. Warfarin is $10 to $30. Insurance often covers DOACs, but prior authorizations can delay things. In the UK’s NHS, DOACs are generally available, but cost isn’t always the deciding factor-safety and convenience are. If you’re paying out of pocket, ask about generic options. Apixaban has generics now. Rivaroxaban might be cheaper through mail-order pharmacies. Don’t let cost stop you, but do talk to your pharmacist about options.What Happens If You Switch Back?
Sometimes, switching back to warfarin is necessary-like if you get pregnant, develop severe kidney failure, or need a mechanical valve. But reversing the switch is even riskier. You can’t just stop the DOAC and restart warfarin. You need to overlap them with a short-acting injectable anticoagulant like heparin until the INR reaches therapeutic levels. This is complex. Only specialists should handle it.Final Takeaway: Do It Right, or Don’t Do It
Switching from warfarin to a DOAC can be one of the best decisions you make for your long-term health. Fewer blood tests, less worry, lower stroke risk. But it’s not a DIY project. It needs expert timing, proper testing, and clear instructions. If your doctor hasn’t walked you through this step-by-step, ask. If they’re not checking your INR before the switch, push back. If they’re not giving you a written plan for missed doses or surgery, request one. Your life depends on getting this right. Don’t assume it’s simple. It’s not. But when done correctly, it’s life-changing.Can I switch from warfarin to a DOAC on my own?
No. Switching requires precise timing based on your INR level, kidney function, and other health factors. Only clinicians experienced in anticoagulation management should make this change. Doing it without medical supervision increases your risk of stroke or dangerous bleeding.
Which DOAC is safest for older adults?
Apixaban is often preferred for older adults, especially those over 75 or with mild kidney impairment. It has the lowest risk of major bleeding among DOACs and doesn’t require as strict a dose adjustment as others. Studies show it’s effective and safer in this group compared to dabigatran or rivaroxaban.
Do I still need blood tests after switching to a DOAC?
You won’t need regular INR tests anymore. But you still need kidney function checks every 6 to 12 months, especially if you’re over 65 or have other health conditions. Some doctors also check liver function and blood counts annually. It’s not routine monitoring-but it’s still necessary.
What should I do if I miss a dose of my DOAC?
If you miss a dose and it’s less than 6 hours past your usual time, take it right away. If it’s more than 6 hours late, skip the missed dose and take your next one at the regular time. Never double up. Missing doses increases your stroke risk, especially if you have atrial fibrillation. Set phone reminders or use a pill organizer.
Can I take NSAIDs like ibuprofen while on a DOAC?
Avoid NSAIDs like ibuprofen or naproxen if possible. They increase your risk of stomach bleeding when combined with DOACs. Use acetaminophen (paracetamol) for pain instead. If you must take an NSAID, talk to your doctor first. They may prescribe a stomach-protecting drug like omeprazole.
Is it safe to switch if I’ve had a recent stroke or clot?
It’s risky. If you’ve had a recent clot or stroke, your doctor may delay switching until your condition stabilizes. Stopping anticoagulation-even briefly-can trigger another event. In these cases, experts recommend continuing warfarin until the risk of recurrence drops, then switching under close supervision.
Why can’t I use DOACs if I have a mechanical heart valve?
DOACs have been tested in people with mechanical valves-and they failed. Studies showed higher rates of valve clots and strokes compared to warfarin. Warfarin is still the only approved option because it’s proven to prevent these dangerous clots on artificial valves. Switching could be deadly.
How do I know if my DOAC dose is right?
Unlike warfarin, there’s no blood test to check DOAC levels. Your dose is based on your kidney function, weight, age, and other medications. If you’re on the correct dose according to your doctor’s guidelines and you’re not bleeding or having clots, it’s likely right. Regular check-ins and kidney tests help confirm it stays safe.






Marian Gilan
26 Jan 2026 at 22:23so i heard from this guy on youtube that DOACs are just a pharma scam to make us buy expensive pills instead of good ol warfarin... and that the inr test is actually a secret way to track us with microchips? idk man but my cousin swears he saw a drone outside his lab last week. 🤔