The VA formulary isn’t just a list of drugs-it’s the backbone of how millions of veterans get affordable, reliable medication. If you’re a veteran enrolled in VA healthcare, you’ve probably noticed that your prescriptions cost far less than what you’d pay elsewhere. That’s not luck. It’s the result of a tightly managed, nationwide system built on one simple rule: use the generic version unless there’s a medical reason not to.
How the VA Formulary Works
The VA National Formulary is mandatory. Every VA clinic, hospital, and pharmacy across the country must carry the same approved medications. There’s no variation between states or regions. This isn’t like commercial insurance, where your plan might cover one drug but not another based on your employer’s contract. The VA formulary is standardized, updated monthly, and publicly available through the VA Formulary Advisor tool.
It’s divided into three tiers, each with a different copay:
- Tier 1: Preferred generics. These are the most cost-effective, clinically proven drugs. Copay is $0-$9 for a 30-day supply.
- Tier 2: Non-preferred generics or some brand-name drugs with generic alternatives available. Copay is $10-$14.
- Tier 3: Brand-name drugs with no generic available, or specialty medications. Copay is $20-$50, depending on the drug and your eligibility.
Most veterans pay nothing for Tier 1 medications. That’s because the VA pushes generics hard-and it works. In 2025, 92% of all prescriptions filled through the VA were generics. That’s higher than any major commercial insurer or Medicare Part D plan.
What’s Covered? Real Examples from the 2025 Formulary
Let’s look at what’s actually on the list. These aren’t theoretical drugs-they’re the ones veterans are using right now:
- Alendronate (for osteoporosis)
- Atorvastatin (for high cholesterol)
- Fluoxetine and Sertraline (for depression and anxiety)
- Hydrochlorothiazide (for high blood pressure)
- Aspirin (buffered, for heart health)
- Allopurinol (for gout)
These are all generics. And they’re all covered at the lowest copay. If your provider prescribes the brand version-say, Zoloft instead of sertraline-the VA will deny the claim unless you’ve been approved for a medical exception. And those exceptions? They’re rare. The VA doesn’t reject brand drugs because they’re expensive. They reject them because the generic works just as well, and studies show it does.
Why Generics? The Science Behind the Policy
Some veterans worry that generics aren’t as good. They’ve heard stories-“My cousin switched to generic and felt worse.” But here’s what the data says:
A 2024 VA Office of Inspector General study tracked 12,450 veterans who switched from brand to generic medications. Of those, 12% initially reported concerns. But after talking to their provider and giving the generic a fair trial, 94% continued using it without issues. Clinical outcomes were identical. Blood pressure, cholesterol, and depression scores didn’t change. Side effects? Same rates.
The VA doesn’t pick generics because they’re cheap. They pick them because they’re proven. The Food and Drug Administration requires generics to have the same active ingredient, strength, dosage form, and bioavailability as the brand. That means they work the same way in your body.
Dr. Susan Turkel, VA’s Chief Consultant for Pharmacy Benefits, put it plainly in the October 2024 newsletter: “We’re not saving money by cutting corners. We’re saving money by using what science says works.” That approach has saved the VA $2.8 billion in 2024 alone.
CHAMPVA and the Limits of Coverage
If you’re a dependent or survivor covered under CHAMPVA (Civilian Health and Medical Program), your formulary is slightly different. In 2025, CHAMPVA expanded coverage for GLP-1 weight-loss drugs-but only for specific FDA-approved uses:
- Mounjaro, Ozempic, Trulicity: Only for type 2 diabetes
- Zepbound: Only for obstructive sleep apnea
- Wegovy: Only for cardiovascular event prevention or metabolic-associated steatohepatitis
That means if your provider wants to prescribe Wegovy for weight loss alone, you’ll need prior authorization-and even then, approval is unlikely. The VA doesn’t cover off-label uses unless there’s strong clinical evidence. This frustrates some veterans, especially those struggling with obesity. But the system is designed to prioritize medications with proven, documented benefits-not trends.
How to Get Your Medications: VA Pharmacy, Meds by Mail, or Community Care
You have three ways to get your prescriptions:
- VA Pharmacy: Pick up at any VA clinic. Bring your VA ID. Most Tier 1 meds are free here.
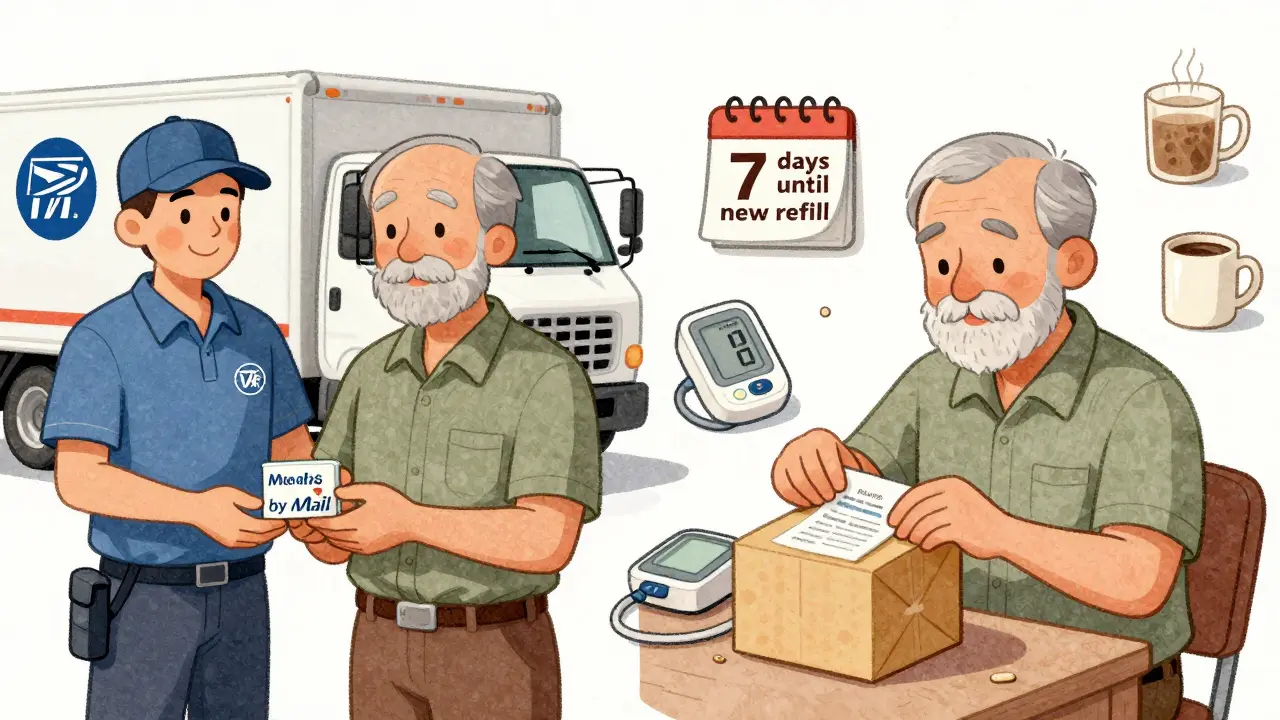
- Meds by Mail: Order 90-day supplies by phone, online, or mail. No copay. No deductible. No shipping fee. This is the most popular option for maintenance meds like blood pressure or diabetes drugs. In 2024, 87% of users rated it “excellent.”
- Community Care: If you’re far from a VA facility or need urgent care, you can fill prescriptions at a network pharmacy. But you must get prior authorization first. Without it, you’ll pay full price.
Pro tip: If you’re on Meds by Mail, don’t forget to refill early. It takes 7-10 days to ship. Running out? Call the VA Pharmacy Benefits line at 1-800-877-8339. They handle 18,000 calls a day and can help fast-track a refill.
What’s Not Covered-and How to Get It
Some newer drugs aren’t on the formulary yet. Think of drugs like Alunbrig (for lung cancer) or Trikafta (for cystic fibrosis). These are expensive. The VA doesn’t automatically cover them. But you can still get them.
Here’s how:
- Ask your provider to submit a prior authorization request. They’ll need to explain why the generic or formulary alternative won’t work.
- Provide clinical evidence-lab results, specialist notes, failed trials.
- Wait 3-7 business days for a decision.
Approval rates for prior authorizations are high-about 80%-if the request is well-documented. But if you just say, “I want the brand,” it’s denied. The VA wants proof, not preference.
How the VA Compares to Other Plans
Let’s put this in perspective. If you’re on Medicare Part D, you’re likely dealing with five tiers, higher copays, and a coverage gap (the “donut hole”). A 30-day supply of atorvastatin might cost you $15-$30. With the VA? $0.
Compare that to commercial insurance. A 30-day supply of sertraline might cost $45 without insurance. With VA? Free. Even with insurance, many people pay $20-$30 for the same drug.
And it’s not just price. The VA formulary is stable. Commercial plans change tiers every year. The VA only adjusts tiers annually, with monthly updates for new drugs or restrictions. That means less confusion. You know what’s covered. You don’t have to guess.

Common Problems and How to Solve Them
Even the best system has hiccups. Here are the top complaints-and how to fix them:
- “I was switched to a generic and I feel different.” Talk to your provider. Don’t stop taking it. Most side effects are temporary. If it’s truly not working, request a therapeutic exception.
- “I can’t find my drug on the formulary.” Use the VA Formulary Advisor. Search by generic name, brand name, or NDC number. If it’s not there, ask your pharmacist to check the Urgent/Emergent Formulary.
- “I got billed for a prescription.” Call the VA Pharmacy Benefits line. Sometimes it’s a system error. You won’t be charged for covered drugs if you’re enrolled.
- “My new drug isn’t approved.” Ask your provider to submit prior authorization. Bring supporting documents. Don’t give up.
New veterans often take 2-3 visits to fully understand the system. That’s normal. Pharmacy staff are trained to help. Ask questions. Take notes. Use the video tutorials on VA.gov.
What’s Coming in 2026
The VA isn’t standing still. In 2026, they’re rolling out AI tools to help providers recommend the best generic alternatives directly in the electronic health record. That means fewer errors, faster decisions, and fewer denials.
They’re also expanding access to rare disease drugs and oncology treatments. Specialty drug costs are rising-12.3% in 2024-but the VA’s growth is slower than the national average. Their long-term plan includes pharmacogenomic testing: using your DNA to predict which drugs will work best for you. That’s not science fiction. It’s already being piloted in a few VA hospitals.
The goal? Keep costs low. Keep care high. Keep veterans healthy.
Are all VA prescriptions free?
No. Most generic medications in Tier 1 cost $0-$9 for a 30-day supply. Tier 2 drugs cost $10-$14, and Tier 3 drugs cost $20-$50. Veterans with service-connected conditions or low income often pay nothing at all. Meds by Mail has no copay for maintenance drugs.
Can I get brand-name drugs through the VA?
Only if there’s a documented medical reason. For example, if you had a severe allergic reaction to the generic, or if clinical studies show the brand is more effective for your condition. You’ll need prior authorization. Otherwise, the VA will only cover the generic version.
How do I check if my drug is covered?
Use the VA Formulary Advisor tool on VA.gov. You can search by drug name, generic name, or NDC number. It shows you the tier, copay, and whether prior authorization is needed. You can also download the full formulary as an Excel file.
What if I need a drug not on the formulary?
Your provider can submit a prior authorization request. They’ll need to explain why alternatives won’t work. Approval rates are high if you provide clinical evidence. For urgent needs, the Urgent/Emergent Formulary may allow temporary access through community pharmacies.
Does the VA cover weight-loss drugs like Wegovy?
Only for specific FDA-approved uses: cardiovascular event prevention, metabolic-associated steatohepatitis, or obstructive sleep apnea. Not for general weight loss. CHAMPVA beneficiaries must meet strict criteria. Prior authorization is required and often denied for off-label use.
Can I use my local pharmacy with VA coverage?
Only if you’re enrolled in Community Care and have prior authorization. Otherwise, you’ll pay full price. Always check with your VA pharmacy first. For routine meds, Meds by Mail is free and easier.
Next Steps for Veterans
If you’re new to VA benefits:
- Log in to VA.gov and link your prescriptions.
- Use the Formulary Advisor to check your current meds.
- Enroll in Meds by Mail for 90-day supplies-it saves time and money.
- Call 1-800-877-8339 if you’re confused. Don’t guess. Ask.
If you’re struggling with a denied prescription:
- Ask your provider to write a detailed letter explaining medical necessity.
- Submit supporting lab results or specialist notes.
- Follow up in 5 days. Don’t wait.
The VA formulary system isn’t perfect. But it’s one of the most effective, transparent, and affordable prescription programs in the country. For veterans, it’s not just about saving money. It’s about making sure you get the right meds-without the hassle, without the surprise bills, without the guesswork.









Babe Addict
27 Dec 2025 at 19:47Yeah right, like the VA actually gives a damn about clinical outcomes. They just want to cut costs so they can buy more drones. I got switched from Lexapro to sertraline and my anxiety went from manageable to ‘why am I crying in the Walmart parking lot?’ Turns out generics don’t always ‘work the same.’ But sure, keep telling yourself it’s science.