Chemo Drug Interaction Checker
Check Your Medication Safety
Enter medications you're taking, and we'll check for potential interactions with common chemotherapy drugs. This tool is for informational purposes only and should not replace professional medical advice.
When someone is diagnosed with cancer, chemotherapy is often one of the first treatments mentioned. It’s not glamorous, but it’s powerful. About 650,000 people in the U.S. alone receive chemotherapy each year in outpatient settings, and more than half of all cancer patients will get it at some point. But here’s the thing: chemotherapy doesn’t work in a vacuum. It interacts with everything else in your body - other medications, supplements, even foods. And those interactions can make the difference between life and death.
How Chemotherapy Actually Works
Chemotherapy isn’t one drug. It’s a whole family of chemicals designed to kill fast-growing cells. That’s why it works on cancer - tumors grow quickly. But it also hits your hair follicles, gut lining, and bone marrow. That’s where the side effects come from: hair loss, nausea, low blood counts.
There are over 100 different chemo drugs, grouped by how they work. Anthracyclines like doxorubicin attack DNA directly but can damage your heart if you get too much - doctors cap lifetime doses at 450-550 mg/m². Alkylating agents like cyclophosphamide mess with DNA repair. Antimetabolites like methotrexate trick cells into using fake building blocks, so they can’t copy themselves. Plant alkaloids like vincristine freeze cell division in place.
Most patients get combinations - not one drug, but three or four. The BEP regimen for testicular cancer uses bleomycin, vinblastine, and cisplatin together. Why? Because cancer cells are sneaky. One drug might kill 90% of the tumor. But the other 10%? They’re the ones that survive and come back stronger. Combine drugs, and you hit them from multiple angles. That’s why 70% of chemo regimens use multiple agents.
Why Drug Interactions Are a Big Deal
Let’s say you’re on chemo and also take ibuprofen for joint pain. Sounds harmless, right? But ibuprofen can interfere with how your kidneys clear certain chemo drugs. That means the chemo sticks around longer - and your body gets hit harder. Same thing with St. John’s wort, a popular herbal supplement. It speeds up liver enzymes that break down chemo. Result? The drug gets cleared too fast. You get less benefit. The cancer might grow.
Even common antibiotics can be dangerous. Some, like erythromycin, slow down the liver’s ability to process chemo. Others, like rifampin, speed it up. Both can be risky. A 2023 study in NEJM Evidence showed that patients on chemo who also took certain antibiotics had a 30% higher chance of severe side effects like low white blood cell counts or kidney damage.
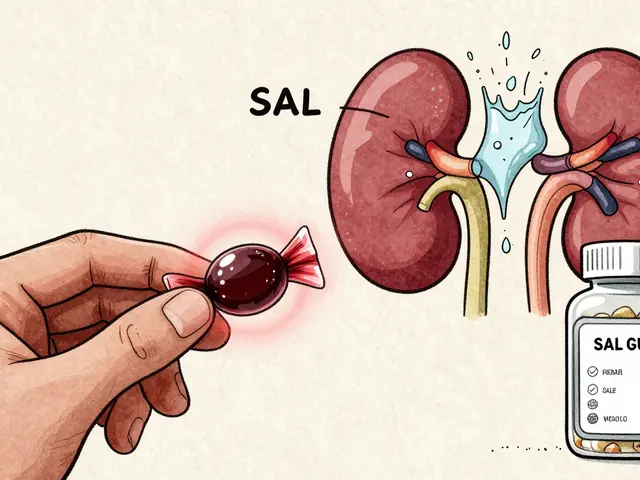
And it’s not just prescription drugs. Over-the-counter painkillers, antacids, vitamins, and even grapefruit juice can change how chemo works. Grapefruit blocks enzymes that break down many chemo drugs - so levels build up dangerously. One glass of juice can affect you for days.
Who’s at Highest Risk?
Not everyone on chemo has the same risk. Older patients, those with kidney or liver disease, and people taking multiple medications are most vulnerable. About 40% of cancer patients over 65 take five or more medications. That’s a recipe for interactions.
Black patients face higher risks too. A 2023 Patient Advocacy Foundation survey found they were 1.7 times more likely to have chemo treatments delayed due to low blood counts - often because their other medications weren’t reviewed properly. It’s not about biology. It’s about gaps in care.
Oral chemo pills are another hidden danger. Patients often forget to take them, or skip doses because they feel sick. Studies show 20-30% of people don’t take oral chemo as prescribed. That’s not laziness - it’s confusion. Some pills need to be taken on an empty stomach. Others must be swallowed whole. One mistake can lower effectiveness or increase toxicity.
What Doctors and Pharmacists Do to Prevent Problems
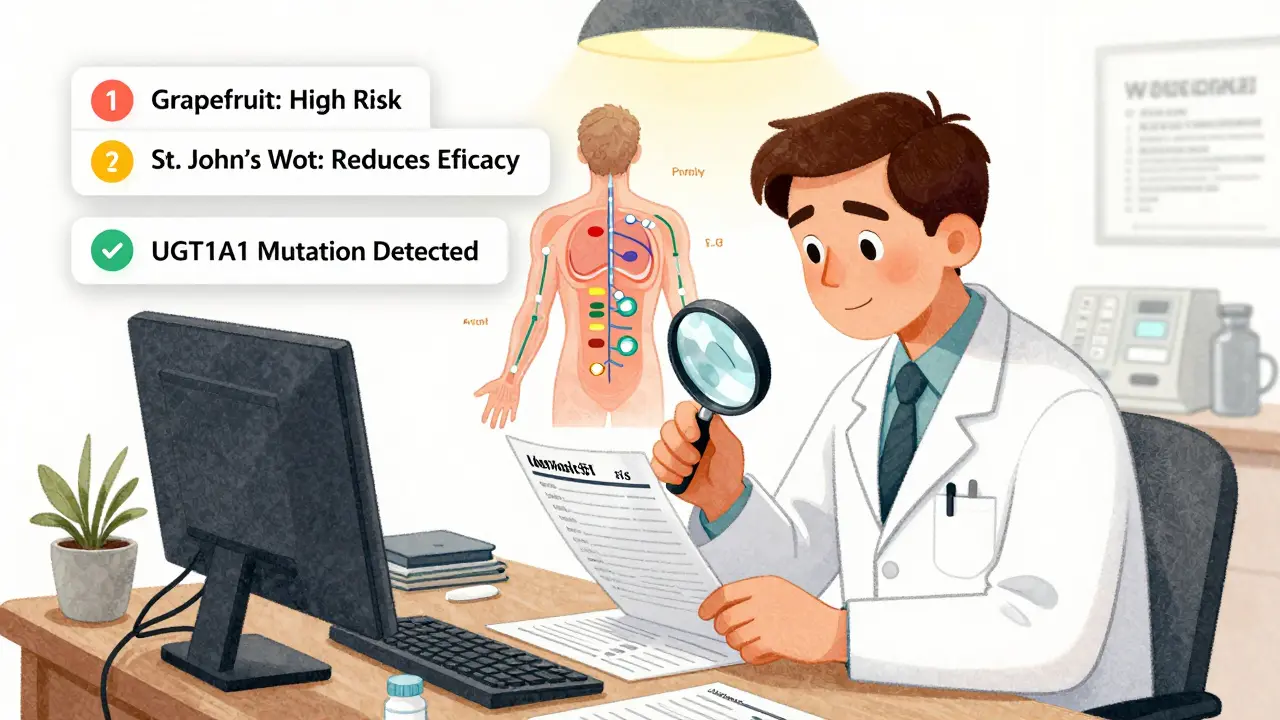
Good cancer centers don’t just hand you a prescription and say, “Good luck.” They have oncology pharmacists - specialists trained in chemo interactions - reviewing every single drug you take. In the U.S., 98% of major cancer centers use them. They check for:
- Drug-drug interactions (like chemo + statins)
- Drug-food interactions (like grapefruit or dairy with certain pills)
- Drug-supplement interactions (like fish oil thinning blood before surgery)
- Genetic risks (like UGT1A1 mutations making irinotecan toxic)
Some drugs come with FDA-mandated safety rules. Pemetrexed, used for lung cancer, requires you to take folic acid and B12 before each dose - or you risk severe toxicity. That’s not optional. That’s life-saving.
Electronic prescribing systems now flag dangerous combos before a doctor even clicks “send.” National Cancer Institute-designated centers use these systems 92% of the time. Community clinics? Only 68%. That gap matters.
Real-Life Consequences
One woman in her 50s, on paclitaxel for breast cancer, started taking turmeric capsules for “inflammation.” Turmeric slows liver metabolism. Her chemo levels spiked. She ended up in the hospital with severe neuropathy - numbness and burning in her hands and feet - that never fully went away.
Another patient took omeprazole (Prilosec) for heartburn while on capecitabine, an oral chemo. Omeprazole changed how the drug was absorbed. His cancer didn’t shrink. His oncologist later found the interaction in his chart - but it was too late.
These aren’t rare cases. In fact, a 2022 study in the Journal of Oncology Pharmacy Practice found that nearly 1 in 4 cancer patients had at least one clinically significant drug interaction during treatment.
What You Can Do
You don’t need to be a scientist to protect yourself. Here’s what works:
- Make a full list - every pill, supplement, vitamin, herb, and even over-the-counter drug. Include dosages and how often you take them.
- Bring it to every appointment - not just your oncologist. Show your pharmacist, your primary care doctor, even your dentist.
- Ask: “Could this interfere with my chemo?” Don’t assume it’s safe just because it’s natural or sold at the grocery store.
- Use one pharmacy - not multiple. That way, one pharmacist can see everything you’re taking.
- Don’t start anything new - not even a new vitamin - without checking with your oncology team.
And if you’re on oral chemo? Set phone alarms. Use pill organizers. Ask for written instructions. If you miss a dose, don’t double up. Call your team. They’ll tell you what to do.
The Future: Smarter Chemo
Chemo isn’t going away - but it’s changing. New drugs like sacituzumab govitecan (Trodelvy) deliver chemo directly to cancer cells using a guided missile system. Less poison in your blood. Fewer side effects.
Doctors are also using blood tests to track tumor DNA. If the cancer is gone from the bloodstream after a few cycles, you might not need all 12 planned treatments. A 2023 trial showed this approach cut unnecessary chemo by 32% without hurting survival.
And genetic testing? It’s becoming standard. Before giving irinotecan, they check your UGT1A1 gene. If it’s slow-metabolizing, they lower the dose. No more life-threatening diarrhea. Before tamoxifen, they test CYP2D6. If you’re a poor metabolizer, tamoxifen won’t work - so they switch you to something else.
These aren’t futuristic ideas. They’re happening now. And they’re making chemo safer - but only if you’re part of the conversation.
Support Matters More Than You Think
Chemotherapy is hard. Fatigue hits 68% of patients. Nausea still affects more than half, even with modern anti-nausea drugs. Peripheral neuropathy from taxanes can last years. But here’s the good news: patients who get integrated palliative care - meaning support for pain, anxiety, and practical help - report 35% higher quality of life and 22% fewer ER visits.
It’s not about giving up. It’s about fighting smarter. If you’re struggling, say so. Ask for help. Ask for a social worker. Ask for nutrition advice. Ask for mental health support. Your team wants to help - but they can’t read your mind.
Can I take over-the-counter painkillers while on chemotherapy?
Some are safe, others aren’t. Tylenol (acetaminophen) is usually okay in standard doses. But NSAIDs like ibuprofen or naproxen can increase bleeding risk or kidney stress, especially with chemo drugs that affect those organs. Always check with your oncology team before taking anything - even a single pill.
Does grapefruit really interfere with chemotherapy?
Yes. Grapefruit blocks enzymes in your liver and gut that break down many chemo drugs. This causes higher levels of the drug in your blood, which can lead to dangerous toxicity. Even a single glass can affect you for up to 72 hours. Avoid grapefruit, Seville oranges, pomelos, and related juices entirely during chemo unless your doctor says otherwise.
Why do I need to take vitamins with some chemo drugs?
Certain chemo drugs, like pemetrexed, cause severe side effects by depleting essential nutrients. That’s why you’re given folic acid and vitamin B12 - not to boost health, but to prevent life-threatening toxicity. These aren’t optional supplements. They’re part of the treatment plan.
Can herbal supplements like turmeric or CBD help with chemo side effects?
Some patients report feeling better, but there’s little proof they help - and a lot of risk. Turmeric slows liver metabolism, which can raise chemo levels dangerously. CBD may interfere with how your body processes certain drugs. No herbal product is regulated like medicine. Always tell your oncologist if you’re using them - and never start without approval.
What should I do if I miss a dose of oral chemotherapy?
Don’t double up. Call your oncology team immediately. Some drugs can be skipped without harm; others require specific adjustments. Taking too much can cause severe toxicity. Missing a dose might reduce effectiveness. Either way, your team needs to know so they can guide you safely.
Are drug interactions worse for older patients?
Yes. Older adults often take multiple medications for other conditions - heart disease, diabetes, arthritis - and their liver and kidneys process drugs slower. This increases the chance of dangerous buildup. That’s why a full medication review is critical before starting chemo, especially for anyone over 65.
Next Steps: Stay in Control
Chemotherapy saves lives. But it’s not magic. It’s medicine - powerful, precise, and easily disrupted. The best way to protect yourself is to be informed and involved. Keep a written list of everything you take. Ask questions. Don’t be shy. Your oncology team is there to help you navigate this - not just treat your cancer, but keep you safe while doing it.
If you’re unsure about a medication, supplement, or even a new food - stop. Call. Wait. Get the answer. Your life depends on it.








Chelsea Harton
18 Jan 2026 at 02:04chemo is wild. one day you’re fine, next day your body feels like it’s been through a meat grinder. and don’t even get me started on grapefruit juice. i thought it was ‘healthy’… turns out it’s like pouring gasoline on a fire. oops.