Statin Myopathy Risk Assessment Tool
Personalized Risk Assessment
This tool helps you understand your risk of statin-induced muscle pain based on key factors discussed in the article.
Your Risk Assessment Results
Millions of people take statins every year to lower their cholesterol and reduce heart attack risk. But for a significant number of them, the benefits come with a painful trade-off: unexplained muscle pain, weakness, or cramps that don’t go away. This isn’t just "getting older" or "being out of shape." It’s statin-induced myopathy-a real, measurable condition that’s more common than most doctors admit.
What Exactly Is Statin-Induced Myopathy?
Statin-induced myopathy isn’t one single problem. It’s a spectrum of muscle damage caused by cholesterol-lowering drugs like atorvastatin, simvastatin, and rosuvastatin. Symptoms usually show up within the first six months of starting the medication. You might feel like your legs are heavy, your calves cramp at night, or you’re too tired to climb stairs-even if you were active before. The scary part? About 1 in 3 people on statins report muscle symptoms. But only a small fraction-less than 1%-have the severe form where muscle enzymes like creatine kinase (CK) spike above 10 times the normal level. Still, even mild symptoms are enough to make people quit their medication. In fact, 72% of patients in one survey stopped taking statins because of muscle discomfort.Why Do Statins Hurt Muscles?
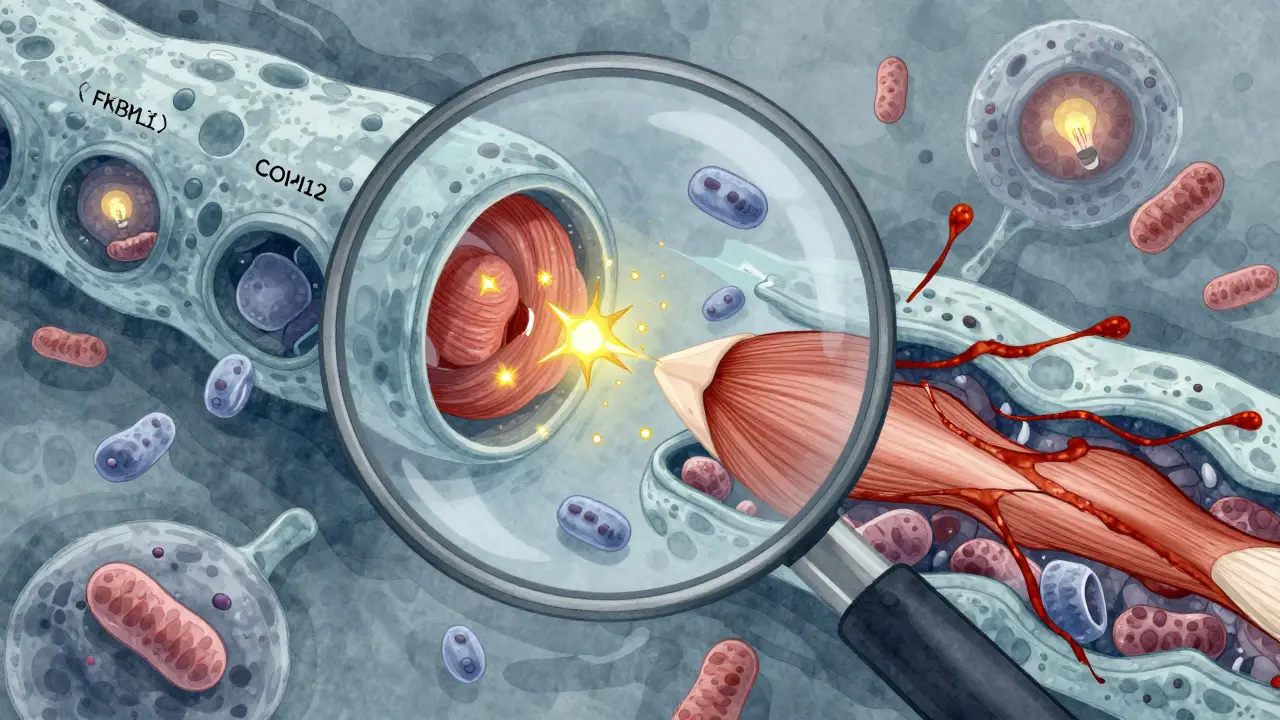
For years, doctors thought statins caused muscle problems simply by lowering CoQ10, a compound your body needs to make energy in muscle cells. That’s true-but it’s only part of the story. Recent research has uncovered three major pathways that work together to damage muscle tissue. First, statins disrupt calcium control in muscle cells. Normally, calcium is tightly regulated inside the sarcoplasmic reticulum, a structure that acts like a battery pack for muscle contraction. Statins cause a protein called FKBP12 to detach from the ryanodine receptor (RyR1), which is the gate that releases calcium. When FKBP12 leaves, the gate leaks. Calcium floods out randomly, triggering muscle spasms, inflammation, and eventually cell death. One study showed this leak increases by 2.3 times in human muscle tissue after statin use. Second, statins block the production of isoprenoids-molecules that help anchor key signaling proteins to cell membranes. Without them, muscle cells can’t communicate properly. This disruption is linked to fatigue and weakness. Third, CoQ10 drops by about 40% in muscle tissue after just four weeks of statin therapy. That means mitochondria-the powerhouses of the cell-struggle to produce energy. As a result, reactive oxygen species build up, causing oxidative stress. Think of it like rust forming inside your muscles. And then there’s the rare but serious autoimmune form. In 5-10% of persistent cases, the body starts making antibodies against HMG-CoA reductase-the very enzyme statins target. This leads to a condition called anti-HMGCR myositis. It’s rare (affecting only 0.02% of statin users), but it’s brutal. Patients often need immunosuppressants like prednisone and methotrexate to stop the immune system from attacking their own muscles.Who’s Most at Risk?
Not everyone on statins gets muscle pain. But some people are far more likely to.- Older adults (especially over 75)
- People with kidney or liver disease
- Those taking multiple medications (like fibrates or certain antibiotics)
- People with hypothyroidism
- Those with a genetic predisposition (like SLCO1B1 gene variants)
- Those who are sedentary
What Should You Do If You Have Muscle Pain?
If you start feeling muscle pain after beginning a statin, don’t just tough it out. Don’t quit cold turkey, either. Follow a smart, step-by-step approach.- Track your symptoms. Note when they started, how bad they are, and whether they get worse with activity.
- Get a blood test. Ask for creatine kinase (CK) levels. If it’s more than 10 times the upper limit, stop the statin immediately.
- Try a washout. Stop the statin for 4 weeks. If your symptoms improve, it’s likely statin-related. In 80% of cases, symptoms fade within this window.
- Rechallenge carefully. Go back on the same statin at a lower dose. If symptoms return, try a different statin. About 40% of people tolerate a switch.
- Try CoQ10. A 2022 European study found 200 mg per day reduced symptoms by 35% in randomized trials. It’s not a magic fix, but it helps many.
- Consider alternatives. Ezetimibe lowers LDL by 20-25% with almost no muscle side effects. PCSK9 inhibitors like evolocumab have only a 3.7% muscle adverse event rate-lower than placebo.
The Exercise Advantage
One of the most overlooked solutions is movement. A 2023 phase II trial showed that combining moderate exercise with CoQ10 supplementation resolved symptoms in 80% of patients. That’s higher than either treatment alone. Why does this work? Exercise seems to restore FKBP12 binding to the RyR1 channel. In animal studies, rats that ran on wheels had normal calcium control even while on statins. Human data confirms it: exercisers had 32% lower CK levels and 41% fewer symptoms than sedentary users. You don’t need to run a marathon. Thirty minutes a day, five days a week-brisk walking, cycling, swimming-makes a measurable difference. And it doesn’t just help your muscles. It protects your heart too.
What’s on the Horizon?
The future of statin therapy isn’t about stopping them-it’s about making them safer. A new drug called S107, which stabilizes the RyR1 channel, reduced muscle symptoms by 52% in a 2023 clinical trial. Two experimental statins-STT-101 and STT-202-are being designed to target the liver while avoiding muscle tissue. In early tests, they showed 70% less penetration into skeletal muscle. Meanwhile, the American College of Cardiology is pushing for better screening before prescribing statins. They now recommend discussing muscle risk upfront. In fact, 78% of cardiologists say they now routinely talk about muscle side effects before starting therapy.Final Reality Check
Statins save lives. They reduce heart attacks, strokes, and death in high-risk patients by up to 30%. But for millions, the muscle pain is real, disabling, and often dismissed. You don’t have to choose between your heart and your muscles. There are smarter ways forward: lower doses, different drugs, CoQ10, exercise, and new therapies on the horizon. The key is recognizing the problem early, not ignoring it. If you’re on a statin and feel weak, sore, or tired for no reason-talk to your doctor. Don’t assume it’s normal. Don’t quit without a plan. And don’t give up on heart health. There’s a better way to manage both your cholesterol and your muscles.Can statins cause permanent muscle damage?
In most cases, no. Muscle symptoms from statins usually resolve within 1-4 weeks after stopping the drug. However, in the rare autoimmune form (anti-HMGCR myositis), muscle damage can persist without treatment. This form requires immunosuppressive therapy and can lead to long-term weakness if not diagnosed early.
Does CoQ10 really help with statin muscle pain?
Yes, for many people. Clinical trials show that 200 mg of CoQ10 daily reduces muscle pain and weakness by about 35%. It works best when combined with moderate exercise. While it doesn’t fix all cases, it’s one of the safest, most evidence-backed options for managing statin-related muscle symptoms.
Should I stop taking statins if I have muscle pain?
Don’t stop without talking to your doctor. Stopping statins can increase your risk of heart attack or stroke, especially if you’re high-risk. Instead, get your creatine kinase tested and try a statin washout. If symptoms improve, you can explore alternatives like lower doses, different statins, or non-statin drugs like ezetimibe or PCSK9 inhibitors.
Is statin myopathy more common in older adults?
Yes. People over 75 are at higher risk, especially if they have kidney issues, take multiple medications, or are inactive. Age-related changes in muscle metabolism and reduced liver clearance of statins make older adults more sensitive to side effects. That’s why doctors now recommend lower starting doses for seniors.
Can exercise prevent statin muscle pain?
Yes. Regular moderate exercise-like walking 30 minutes five days a week-has been shown to reduce muscle symptoms by nearly 60%. Exercise helps stabilize the calcium channels in muscle cells that statins disrupt. It’s one of the few interventions that targets the root cause, not just the symptoms.
Are there statins that don’t cause muscle pain?
No statin is completely free of muscle side effects, but some are better tolerated. Pravastatin and fluvastatin tend to cause fewer muscle problems than simvastatin or atorvastatin. Newer non-statin drugs like ezetimibe and PCSK9 inhibitors have muscle adverse event rates lower than placebo, making them good alternatives for those who can’t tolerate statins.







Ayush Pareek
15 Jan 2026 at 20:10Been on statins for 5 years. Muscle cramps got bad enough I almost quit. Started walking 30 mins daily and took 200mg CoQ10. Within 3 weeks, the heaviness in my legs was gone. Not magic, but real. Don’t let doctors dismiss it - you’re not lazy, your muscles are just stressed.