When your lungs start to feel heavy, your cough won’t quit, and even breathing feels like a chore, it’s not just a cold. It could be pneumonia - and not all pneumonia is the same. The kind you get depends on what’s attacking your lungs: bacteria, viruses, or fungi. Each one acts differently, shows up differently, and needs a totally different treatment. Getting it wrong can mean wasted time, unnecessary antibiotics, or even life-threatening complications.
Bacterial Pneumonia: The Sudden Onset
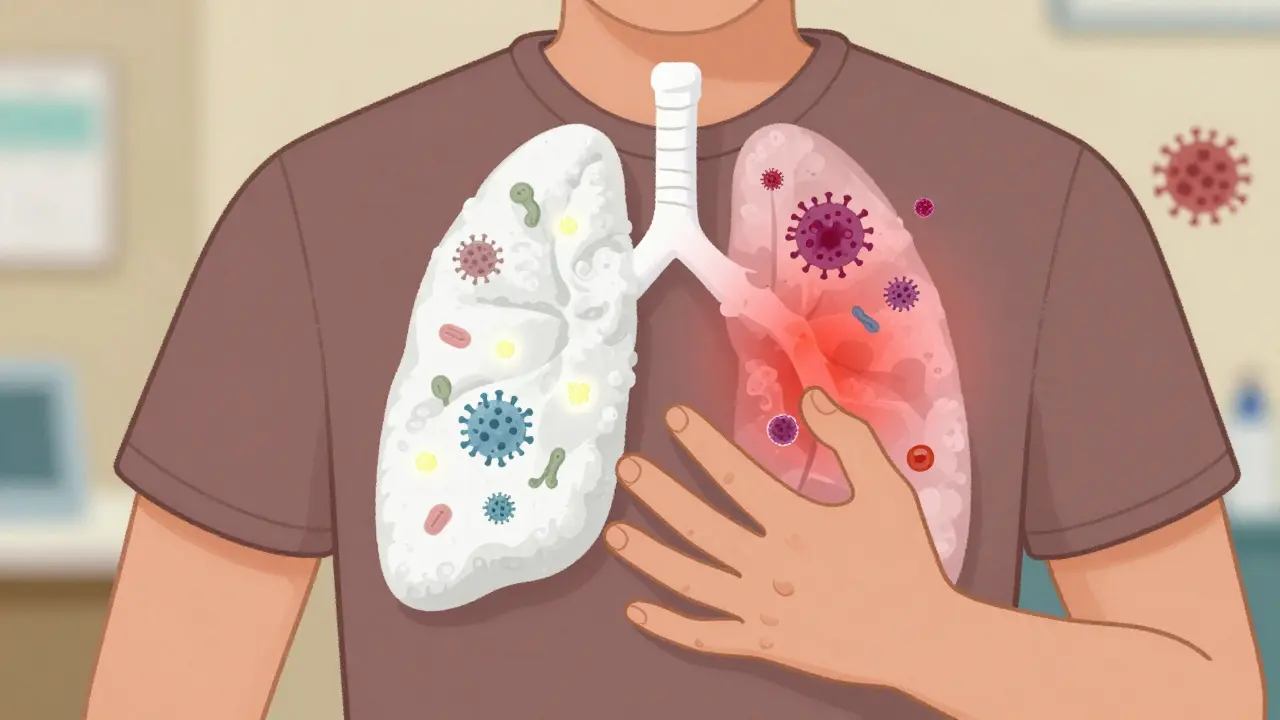
Bacterial pneumonia hits fast. One day you might feel fine; the next, you’re running a high fever - 102°F to 105°F - with chills, sharp chest pain, and a cough that brings up thick, yellow or green mucus. You might notice your lips or fingernails turning slightly blue because your body isn’t getting enough oxygen. This isn’t just a bad cough. It’s your lungs filling up with pus and fluid.
The most common culprit? Streptococcus pneumoniae. It’s responsible for about half of all community-acquired pneumonia cases in the U.S. and around the world. Other bacteria like Haemophilus influenzae, Staphylococcus aureus, and Mycoplasma pneumoniae (which causes "walking pneumonia") also play big roles. Legionella pneumophila, the bug behind Legionnaires’ disease, is rarer but more dangerous, often linked to contaminated water systems.
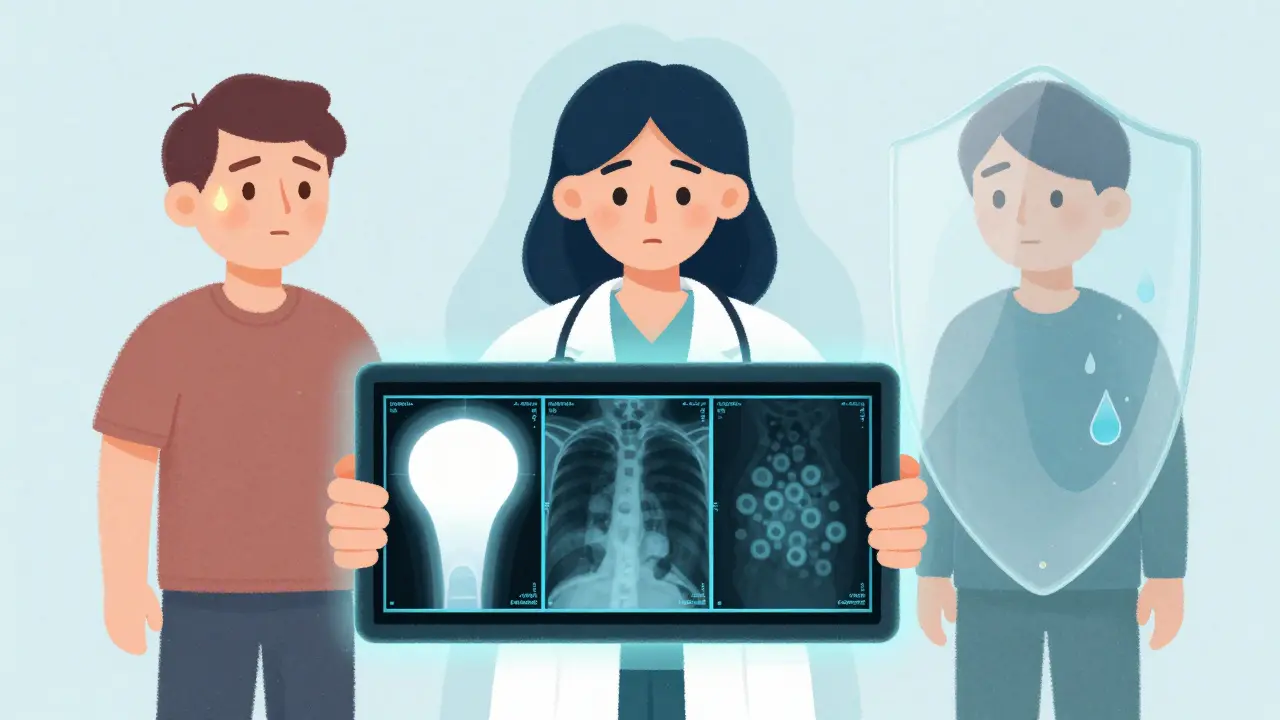
On a chest X-ray, bacterial pneumonia shows up as a solid, white patch - usually on one side of the lung. That’s called lobar consolidation. It means the air sacs (alveoli) are packed with bacteria and immune cells. Your body sends in neutrophils, the first responders of your immune system, to fight the infection. That’s what causes the thick mucus and fever.
Treatment? Antibiotics. Penicillin, amoxicillin, or macrolides like azithromycin work well for most cases. But here’s the catch: if you take antibiotics for something that’s not bacterial, you’re not helping yourself. You’re just making bacteria stronger. The CDC says about 30% of outpatient antibiotic prescriptions are unnecessary - and pneumonia is one of the top reasons why.
Viral Pneumonia: The Slow Burn
Viral pneumonia creeps in. It starts like the flu: sore throat, runny nose, a scratchy cough, maybe a low-grade fever. Then, over three to five days, it settles deeper into your lungs. You feel more tired. Your cough gets worse. You might have muscle aches and headaches. But you usually don’t cough up thick mucus - it’s more of a dry, irritating cough.
The usual suspects? Influenza A and B, RSV (especially in kids and older adults), SARS-CoV-2 (COVID-19), and even common cold viruses like rhinovirus. During flu season, influenza causes about 20-30% of viral pneumonia cases. COVID-19 can lead to pneumonia too, especially in unvaccinated or high-risk people.
On an X-ray, viral pneumonia looks totally different. Instead of one solid white patch, you’ll see a hazy, scattered pattern across both lungs. That’s called interstitial infiltrates - inflammation in the tissue around the air sacs, not inside them. Your immune system is working hard, but it’s not sending in the same kind of troops as it does for bacteria.
Antibiotics won’t help here. Treatment is mostly rest, fluids, and fever reducers. In severe cases, especially with flu or COVID-19, antivirals like oseltamivir or remdesivir can shorten the illness if given early. But here’s the real danger: viral pneumonia often opens the door for a second infection - bacterial pneumonia. About 25-30% of people with severe flu end up with a bacterial superinfection, usually from Streptococcus pneumoniae or Staphylococcus aureus. That’s why doctors watch closely after a viral illness gets worse.
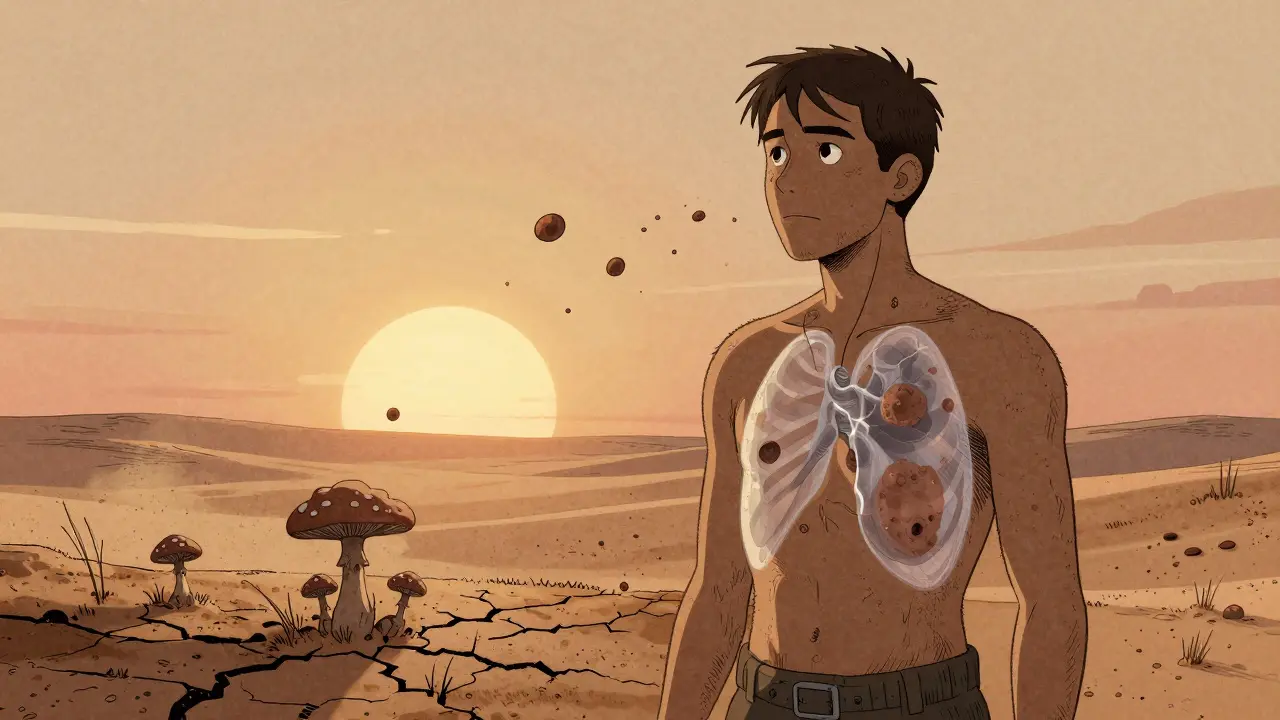
Fungal Pneumonia: The Hidden Threat
Fungal pneumonia is rare - less than 5% of cases - but it’s serious. And it doesn’t strike healthy people. It targets those with weakened immune systems: people with HIV/AIDS, those on chemotherapy, organ transplant recipients, or anyone taking long-term steroids. If you’re healthy, you breathe in fungal spores all the time. Your body handles them. If your immune system is down, they take root in your lungs.
The three main fungi in the U.S. are Coccidioides (Valley fever), Histoplasma capsulatum (histoplasmosis), and Blastomyces dermatitidis (blastomycosis). You don’t catch them from other people. You breathe them in from soil - especially where there’s bird or bat droppings. Farmers, landscapers, construction workers, and cave explorers are at higher risk. In places like the Southwest (Arizona, California) or the Ohio River Valley, exposure is common.
Symptoms? Fever, cough, chest pain, fatigue - sounds a lot like bacterial or viral pneumonia. But fungal pneumonia can also cause night sweats, weight loss, and even skin rashes or joint pain. It’s sneaky. A chest X-ray might look like bacterial pneumonia, or it might show nodules or cavities. You can’t tell just by looking. You need a special test - a sputum culture, blood test, or biopsy - to find the fungus.
Antibiotics? Useless. Antivirals? No help. You need antifungals: fluconazole, itraconazole, or for severe cases, amphotericin B. Treatment can last months. And even then, relapse is common in people with ongoing immune problems.
How to Tell Them Apart
It’s not always easy - symptoms overlap. But here’s a quick guide:
- Onset: Bacterial = sudden. Viral = gradual. Fungal = slow, often over weeks.
- Fever: Bacterial = high (102°F+). Viral = mild to moderate (100-102°F). Fungal = low-grade or intermittent.
- Cough: Bacterial = wet, colored mucus. Viral = dry or light mucus. Fungal = dry or bloody.
- X-ray: Bacterial = one white patch. Viral = hazy, both lungs. Fungal = nodules, cavities, or patchy.
- Risk: Bacterial = all ages. Viral = kids, elderly, unvaccinated. Fungal = immunocompromised, exposure to soil/dust.
Doctors now use faster tests - multiplex PCR panels - that can check for 20+ viruses and bacteria from one nasal swab. Results in hours. That’s a big step forward. But in many places, especially outside hospitals, diagnosis still relies on symptoms and X-rays.
Prevention: Know What Works
Not all pneumonia is preventable, but many cases are.
Bacterial: The pneumococcal vaccine (Prevnar 20 or Pneumovax 23) cuts risk by 60-70% in kids and 45-75% in adults. But only 68% of adults over 65 are vaccinated. That’s too low. Kids get their first dose at two months - stick to the schedule.
Viral: The flu shot reduces pneumonia risk by 40-60% in good match years. The COVID-19 vaccine cuts pneumonia risk by up to 90% in the first few months after vaccination. Annual shots matter.
Fungal: No vaccine exists. Avoiding dust in endemic areas helps. If you’re immunocompromised and live in or travel to high-risk zones (Arizona, California, Ohio River Valley), wear a mask during outdoor work or in dusty environments. Wash hands after gardening. Don’t ignore symptoms if you’re at risk.
Why It Matters
Pneumonia causes 50,000 deaths in the U.S. every year. Bacterial pneumonia has a 5-7% death rate in hospitalized patients. Fungal pneumonia kills 10-15% of those who get it - especially if diagnosis is delayed. Viral pneumonia, while usually less deadly, can lead to long-term lung damage or trigger deadly secondary infections.
But the biggest hidden cost? Antibiotic misuse. When viral pneumonia is mistaken for bacterial - and antibiotics are prescribed anyway - it doesn’t help the patient. It just fuels drug-resistant superbugs. The CDC says this practice increases resistance by 35% in communities.
Knowing the difference isn’t just about treatment. It’s about protecting yourself, your family, and the future of medicine.
When to See a Doctor
Call a doctor if you have:
- Fever above 102°F that won’t break
- Coughing up blood or thick, colored mucus
- Shortness of breath at rest
- Chest pain that gets worse when you breathe or cough
- Blue lips or fingernails
- Confusion or dizziness (especially in older adults)
Don’t wait for symptoms to get worse. Pneumonia can turn serious fast - especially in kids, older adults, and people with chronic illnesses like COPD, diabetes, or heart disease.
Can you have pneumonia without a fever?
Yes, especially in older adults or people with weakened immune systems. They might only show signs like confusion, fatigue, or a drop in body temperature instead of a fever. This is called "atypical pneumonia" and can be harder to spot.
Is viral pneumonia contagious?
Yes. Viral pneumonia is usually caused by viruses that spread through coughs, sneezes, or touching contaminated surfaces. You can catch the virus that leads to pneumonia before the lung infection fully develops. That’s why handwashing and masks during flu season matter.
Can fungal pneumonia spread from person to person?
No. Fungal pneumonia isn’t contagious. You get it by breathing in spores from the environment - soil, bird droppings, decaying wood. You can’t catch it from someone else, even if they’re sick.
How long does pneumonia last?
Bacterial pneumonia improves in 1-3 weeks with antibiotics. Viral pneumonia can take 2-4 weeks to clear, even without treatment. Fungal pneumonia often needs months of medication, and recovery depends heavily on your immune system. Fatigue can linger for weeks after the infection is gone.
Are there vaccines for all types of pneumonia?
No. Vaccines exist for bacterial pneumonia (pneumococcal) and viral pneumonia (flu, COVID-19). There’s no vaccine for fungal pneumonia. Prevention relies on avoiding exposure, especially if you’re immunocompromised.
Can pneumonia cause long-term lung damage?
Yes. Severe pneumonia, especially viral or fungal, can scar lung tissue. This can lead to reduced lung function, chronic cough, or shortness of breath even after recovery. People with pre-existing lung disease are at higher risk.
Understanding your type of pneumonia isn’t just about getting the right medicine. It’s about knowing how to protect yourself, when to act, and why some treatments don’t work - and why others are life-saving.







Scottie Baker
13 Jan 2026 at 16:06Bro, I had bacterial pneumonia last year and thought I was just dealing with a bad cold. Then I woke up coughing up green slime like a dragon with a sinus infection. Antibiotics saved my ass, but I almost died because I waited too long. Don’t be me.