Blood Thinner & Antiviral Interaction Checker
Select Your Medication
Guidance Summary
Select your medications to view personalized guidance
How to Use This Tool
This tool provides guidance based on current clinical recommendations. Always consult your doctor or pharmacist before making any changes to your medication regimen.
When COVID-19 Changes How Your Blood Thinner Works
If you’re on a blood thinner like apixaban, rivaroxaban, or warfarin and catch a respiratory infection like COVID-19, your medication might suddenly become too strong-or not strong enough. This isn’t theoretical. It’s happening in hospitals and homes across the UK and the US right now. In fact, during the peak of the pandemic, nearly one in three hospitalized COVID-19 patients received therapeutic anticoagulation to prevent deadly clots. But mixing these drugs with common antivirals like Paxlovid can turn a stable treatment into a medical emergency.
The problem isn’t the infection itself. It’s what the infection triggers in your body-and how your meds react to the drugs used to treat it. When SARS-CoV-2 hits your lungs, your blood starts clotting abnormally. Tiny clots form in the lungs, heart, and kidneys. That’s why doctors started giving higher doses of blood thinners to seriously ill patients. But then came the antivirals. And that’s where things got complicated.
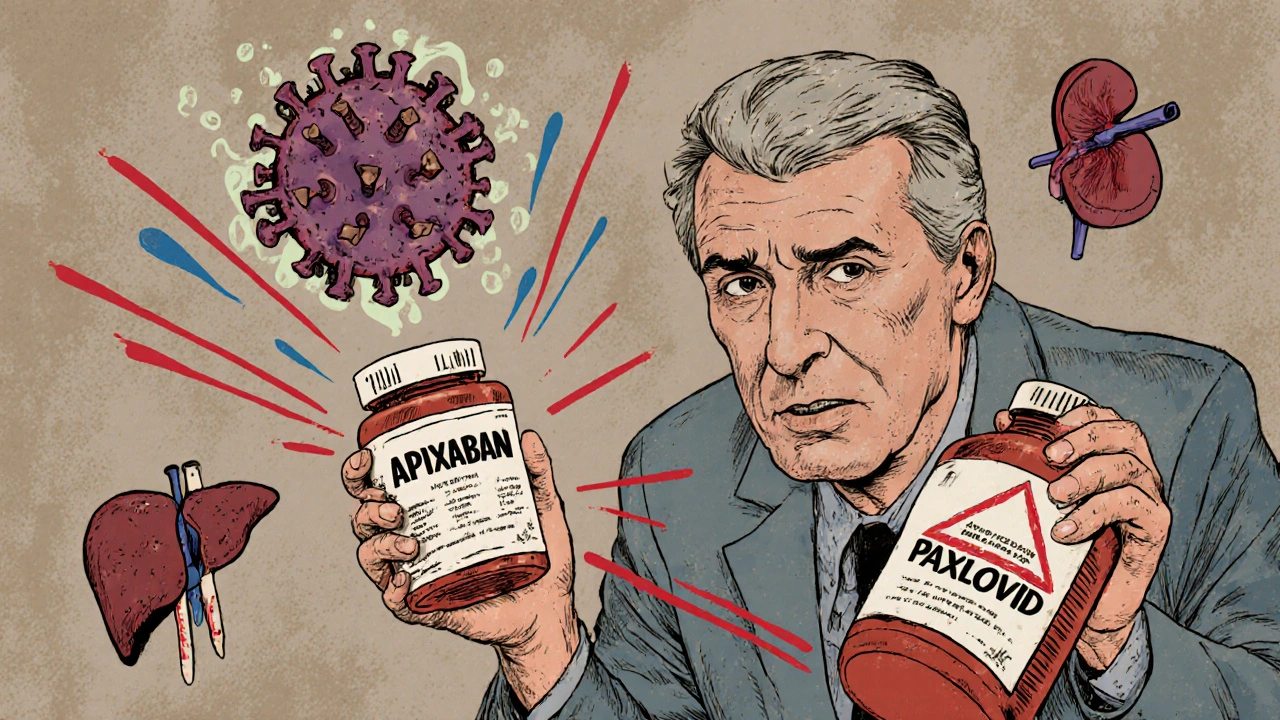
Why Paxlovid Is a Problem for Blood Thinners
Paxlovid, the antiviral combo of nirmatrelvir and ritonavir, works by blocking the virus’s ability to replicate. But ritonavir, the helper drug, is a powerful inhibitor of CYP3A4 and P-glycoprotein-two key systems your liver and gut use to break down medications. And guess what? Most direct oral anticoagulants (DOACs) rely on these same systems to be cleared from your body.
When you take Paxlovid while on rivaroxaban or apixaban, your body can’t process the blood thinner properly. Levels can spike by 3 to 5 times. That’s not a small increase. That’s enough to cause major bleeding-stomach bleeds, brain bleeds, even fatal internal bleeding. A 2023 FDA safety alert documented 147 cases of major bleeding linked to this interaction in just 18 months.
And it’s not just Paxlovid. Older antivirals like lopinavir/ritonavir had the same effect. Even dexamethasone, a steroid used to calm lung inflammation in severe COVID-19, can do the opposite: it speeds up the breakdown of DOACs, dropping their levels by up to 50%. That means you’re suddenly at risk for clots again-pulmonary embolism, stroke, heart attack.
DOACs vs. Warfarin: Which Is Safer During COVID-19?
Not all blood thinners are created equal when it comes to drug interactions.
DOACs (apixaban, rivaroxaban, dabigatran, edoxaban) are convenient-no regular blood tests, fixed doses. But they’re vulnerable to interactions. The FDA and EMA don’t even agree on how to handle them with Paxlovid. In the US, guidelines often say: stop DOACs entirely during the 5-day Paxlovid course. In Europe, some recommend reducing the dose. There’s no universal standard.
For example:
- Rivaroxaban: US guidelines say stop it. EMA says cut the dose in half if kidney function is normal.
- Dabigatran: In the US, avoid it completely if your kidney clearance is below 30 mL/min. In Europe, you might get a reduced dose (75 mg twice daily) if timed correctly.
- Apixaban: Often held for 5 days during Paxlovid, then restarted 2 days after.
Warfarin is different. It doesn’t rely on CYP3A4. But it does need regular INR checks-and COVID-19 messes with those numbers too. Steroids like dexamethasone can make warfarin stronger. Some antivirals can interfere with vitamin K absorption. So while warfarin avoids the CYP3A4 trap, it creates another: unpredictable INR swings. One case study showed a patient’s INR jump from 2.5 to 4.8 after starting dexamethasone and azvudine. That’s a bleeding risk.
Bottom line: Neither is perfect. DOACs are easier to manage normally but risk dangerous interactions. Warfarin is harder to monitor but has fewer direct drug clashes. The choice depends on your kidney function, clotting risk, and what antivirals you’re taking.
Real-World Mistakes and How to Avoid Them
These aren’t just textbook cases. They’re happening in pharmacies, ERs, and homes.
A Reddit user shared a story from August 2022: a 68-year-old man on full-dose rivaroxaban took Paxlovid for COVID-19 and ended up in the hospital with a GI bleed. He needed two units of blood. He didn’t know to stop his blood thinner.
At Mayo Clinic, anticoagulation-related ER visits jumped 37% in the first year of the pandemic. About 28% of those were due to drug interactions. Community pharmacists in the US reported encountering at least one major interaction per month on average. Dabigatran and Paxlovid made up 42% of those cases.
Here’s what actually works:
- Don’t guess. If you’re on a DOAC and get COVID-19, contact your doctor or pharmacist before taking any antiviral.
- Hold the DOAC. For most DOACs, pause during the 5-day Paxlovid course. Restart 2 days after the last dose.
- Consider bridging. If you’re at high risk for clots (e.g., history of DVT, atrial fibrillation with CHA₂DS₂-VASc score ≥3), your doctor might switch you to daily low-molecular-weight heparin (like enoxaparin) during the Paxlovid window.
- Monitor closely. After restarting your DOAC, check for signs of bleeding-unusual bruising, dark stools, headaches, dizziness. If you’re on warfarin, get an INR test within 3 days of restarting antivirals or steroids.
There’s a tool that’s saved thousands of lives: the Liverpool COVID-19 Drug Interactions Checker. Updated daily, it’s used by over 100,000 healthcare providers worldwide. Type in your meds and the antiviral-it tells you exactly what to do.
What Happens After You Recover?
Even after you feel better, the risk doesn’t disappear. Your blood stays in a hypercoagulable state for weeks. Johns Hopkins found that 65% of patients still had elevated D-dimer levels-signs of clotting activity-14 to 21 days after leaving the hospital.
The American Society of Hematology recommends continuing therapeutic anticoagulation for at least 7 days after discharge. For high-risk patients, some experts extend it to 30 days. That’s not just for people who were hospitalized. Even those treated at home with Paxlovid may need extended anticoagulation if they had severe symptoms or have other clotting risks.
And here’s the catch: if you stopped your DOAC during Paxlovid, restarting it too soon can cause bleeding. Waiting too long can cause clots. Timing matters. Your doctor needs to weigh your clotting risk against your bleeding risk. That’s why follow-up is non-negotiable.
What’s Next? New Drugs, Better Tools
The good news? The industry is responding.
Pfizer is already testing its next-generation antiviral, PF-07817883, which doesn’t inhibit CYP3A4. Early results show it’s just as effective as Paxlovid but with far fewer drug interactions. If approved, it could replace Paxlovid within the next few years.
Meanwhile, AI is helping. A 2023 study in Nature Medicine trained a machine learning model on over 12,000 patient records. It predicted the severity of anticoagulant-COVID-19 drug interactions with 89.4% accuracy. That kind of tool could one day be built into electronic health records, warning doctors before a prescription is even written.
Point-of-care testing is improving too. New devices can measure DOAC levels at the bedside in under 15 minutes. No more waiting days for a lab result. That’s huge for emergency situations.
But for now, the responsibility falls on you and your care team. Don’t assume your pharmacist knows your full med list. Don’t assume your doctor remembers you’re on a blood thinner. Be the one who asks: "Is this antiviral safe with my blood thinner?"
Frequently Asked Questions
Can I take Paxlovid if I’m on apixaban?
The safest approach is to stop apixaban for the full 5 days of Paxlovid treatment. Restart it 2 days after your last Paxlovid dose. If you’re at high risk for clots (e.g., recent DVT, mechanical heart valve, or CHA₂DS₂-VASc score ≥3), your doctor may prescribe daily enoxaparin injections during those 5 days as a bridge. Never adjust your dose without medical advice.
Does dexamethasone affect blood thinners?
Yes. Dexamethasone speeds up the breakdown of DOACs like rivaroxaban and apixaban, potentially cutting their effectiveness by up to 50%. This raises your risk of clots. For warfarin, it can make the drug stronger, increasing bleeding risk. If you’re on dexamethasone and a blood thinner, your INR or anti-Xa levels need to be checked more often-ideally every 2-3 days during treatment.
Is warfarin safer than DOACs during COVID-19?
It’s not safer-it’s different. Warfarin doesn’t interact with CYP3A4 like DOACs do, so it avoids the biggest risk with Paxlovid. But it’s more sensitive to diet, other meds, and illness. Infections like COVID-19 can cause wild INR swings. You’ll need frequent blood tests. For many, DOACs are still preferred if they can be managed safely with temporary holds or bridging.
What should I do if I’m on dabigatran and get COVID-19?
In the US, avoid dabigatran with Paxlovid if your kidney clearance is below 30 mL/min. If it’s higher, some experts recommend reducing the dose to 75 mg twice daily and taking it at least 12 hours before or after Paxlovid. But this is high-risk. Many providers prefer switching to enoxaparin for the 5-day course. Always consult your doctor-never adjust on your own.
How long should I stay on blood thinners after COVID-19?
At least 7 days after discharge, according to ASH guidelines. For patients with severe illness, high clotting risk, or elevated D-dimer levels, some experts recommend continuing for up to 30 days. If you were hospitalized, ask your doctor about follow-up D-dimer testing and whether you need longer-term anticoagulation. Don’t assume you’re safe just because you feel better.
Next Steps: What to Do Today
If you’re on a blood thinner:
- Make sure your doctor and pharmacist have your full medication list-including supplements and OTC drugs.
- Save the Liverpool COVID-19 Drug Interactions website on your phone. It’s free and updated daily.
- Ask your provider: "What’s my plan if I get COVID-19?" Get it in writing.
- If you’re prescribed Paxlovid or another antiviral, confirm whether you need to stop or adjust your blood thinner before taking the first dose.
- Watch for bleeding signs: nosebleeds that won’t stop, red or black stools, sudden headaches, unexplained bruising.
Respiratory infections are common. Blood thinners save lives. But when they collide, the stakes are high. Knowledge isn’t just power-it’s protection. Stay informed. Ask questions. Don’t let a simple mistake turn a treatable illness into a life-threatening one.








Christopher Robinson
20 Nov 2025 at 09:11This is the kind of post that saves lives. I’m on apixaban and just got Paxlovid last week-called my pharmacist before taking it. They told me to hold the apixaban and use enoxaparin. Thank you for making this so clear. 🙏💊