Statin Safety Checker
Check if your statin and other medications interact dangerously. This tool analyzes your combination and provides safety recommendations.
Statins save lives. Millions of people take them every day to lower cholesterol and prevent heart attacks and strokes. But for some, the cost is muscle pain - sometimes severe enough to stop the medication altogether. And when statins are mixed with other drugs, that risk can spike dramatically. This isn’t rare. It’s predictable. And it’s preventable.
Why Some Statins Are Riskier Than Others
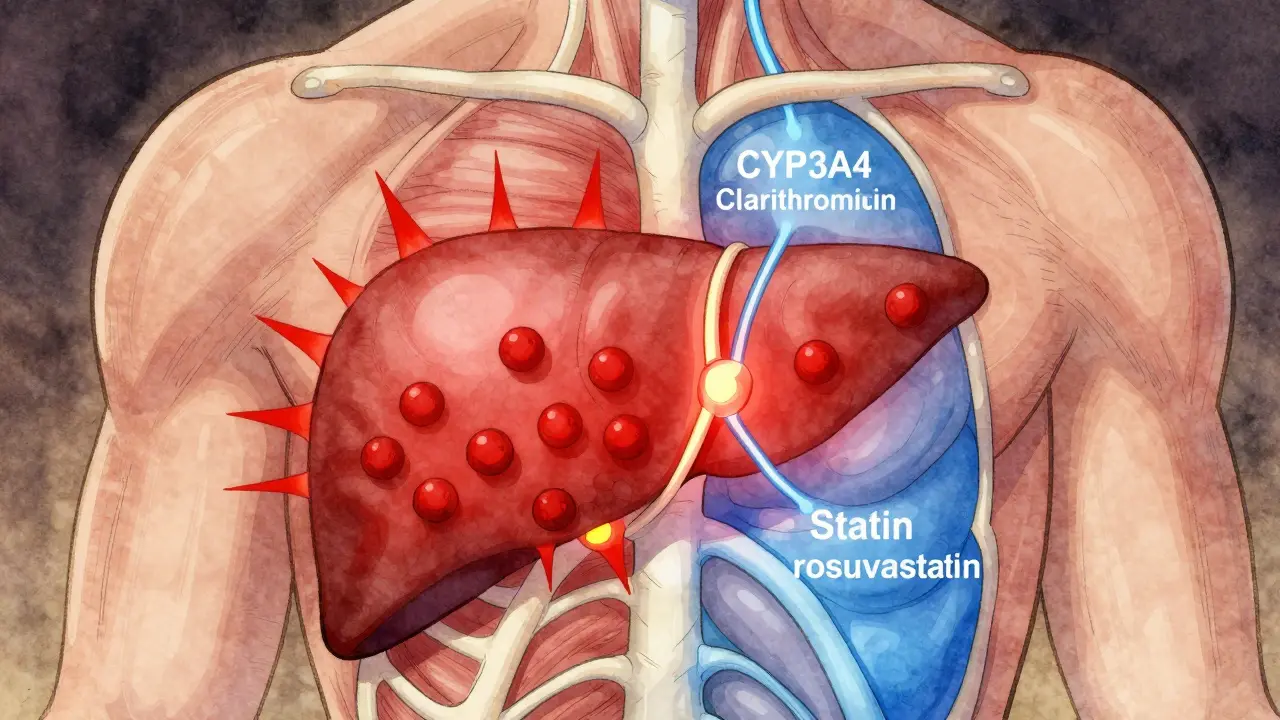
Not all statins are created equal. Some are more likely to cause muscle damage, especially when combined with other medications. The difference comes down to how they’re processed by your liver. Simvastatin and lovastatin are metabolized mostly by the CYP3A4 enzyme. That means if you take a drug that blocks this enzyme - like clarithromycin or erythromycin - your statin levels can jump by 10 times or more. That’s not a small increase. It’s a red flag. Atorvastatin is also affected, but less so. About 70% of it goes through CYP3A4, so interactions still happen, but they’re usually milder. On the other end, pravastatin, rosuvastatin, and fluvastatin barely touch CYP3A4. They’re cleared through different pathways, making them much safer to combine with common antibiotics, antifungals, or blood pressure meds. Here’s the kicker: lipophilic statins (simvastatin, atorvastatin, lovastatin) also soak into muscle tissue more easily than hydrophilic ones (pravastatin, rosuvastatin). Animal studies suggest this increases the chance of muscle damage. Human data confirms it - patients on simvastatin report muscle pain more often than those on pravastatin.Top Medications That Boost Myopathy Risk
Certain drugs are known troublemakers when taken with statins. The biggest offenders:- Clarithromycin and erythromycin: These macrolide antibiotics can raise simvastatin levels by 10-fold. Azithromycin? No problem. It doesn’t block CYP3A4.
- Cyclosporine: Used after transplants, this drug can boost statin levels by 3 to 13 times. It’s one of the most dangerous combinations.
- Gemfibrozil: A fibrate for triglycerides. It doubles statin levels and increases myopathy risk by up to 5 times. Fenofibrate? Much safer.
- Diltiazem and verapamil: Calcium channel blockers for high blood pressure. Both interfere with statin clearance. The FDA now limits simvastatin to 20mg max when taken with these.
- Amiodarone: An anti-arrhythmic. It’s a slow burner - the interaction builds over weeks. That’s why many patients don’t realize the problem until it’s too late.
Who’s Most at Risk?
It’s not just about the drugs. Your body matters too. Seven major risk factors make muscle damage more likely:- Age over 75
- Small body frame or low BMI
- Chronic kidney disease
- Hypothyroidism (underactive thyroid)
- Heavy alcohol use
- Intense physical activity - especially if you’re not used to it
- Genetic variations in the SLCO1B1 gene
What Does Myopathy Actually Feel Like?
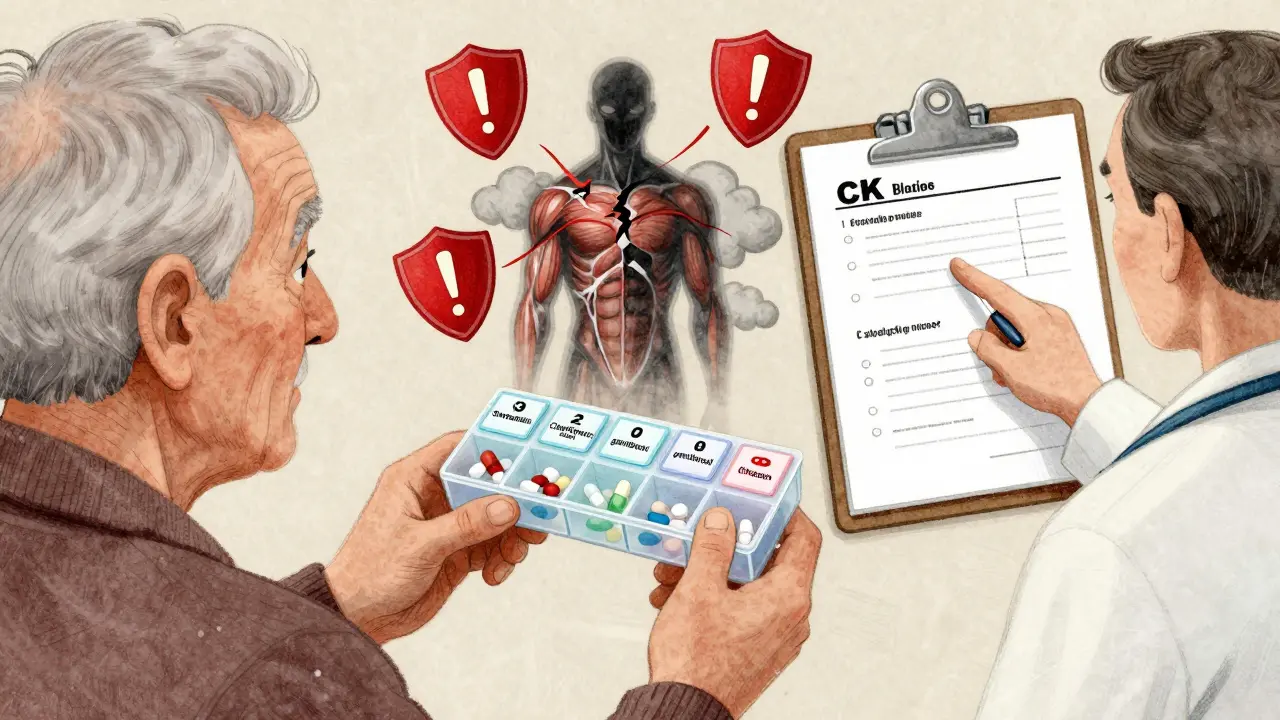
Myopathy isn’t just sore muscles after a workout. It’s persistent, unexplained pain or weakness that doesn’t go away. You might feel like you’re dragging your legs. Climbing stairs becomes hard. Lifting your arms feels heavy. The real danger comes when it turns into rhabdomyolysis. That’s when muscle fibers break down and spill into your blood. Myoglobin - the protein inside muscles - floods your kidneys. That can cause kidney failure. It’s rare, but it’s deadly. Doctors look for two things: symptoms and blood tests. Muscle pain or weakness, plus a creatine kinase (CK) level more than 10 times the normal upper limit. That’s the diagnostic cutoff. If your CK is 5x above normal and you have symptoms, most guidelines say to stop the statin.What to Do If You Have Muscle Pain
Don’t ignore it. Don’t assume it’s just aging. Don’t stop the statin on your own - but do call your doctor. Here’s what to ask for:- A CK blood test. Baseline before starting a new statin. Repeat if pain starts.
- A review of every medication you take - including over-the-counter pills, supplements, and herbal products.
- A switch to a safer statin. Pravastatin or rosuvastatin (at 10-20mg) are top choices for people with muscle issues.
- A dose reduction. Sometimes, cutting simvastatin from 80mg to 20mg cuts the risk dramatically.
Alternatives When Statins Don’t Work
If you’ve tried multiple statins and still get muscle pain, you’re not out of options. Bempedoic acid (Nexletol) is the newest. It lowers LDL cholesterol without entering muscle cells. That’s why it doesn’t cause myopathy. But it costs over $4,000 a year. Generic atorvastatin? About $6.60. Price matters. Icosapent ethyl (Vascepa) is another option. It’s not a statin - it’s a purified fish oil. The STRENGTH trial showed it reduces heart attacks and strokes in people already on statins. It’s not a replacement, but it can help lower the statin dose you need. Coenzyme Q10 supplements are often recommended. The evidence is weak, but some patients swear by them. If you want to try it, 100-200mg daily is the usual dose. No harm in it, as long as you’re not expecting miracles.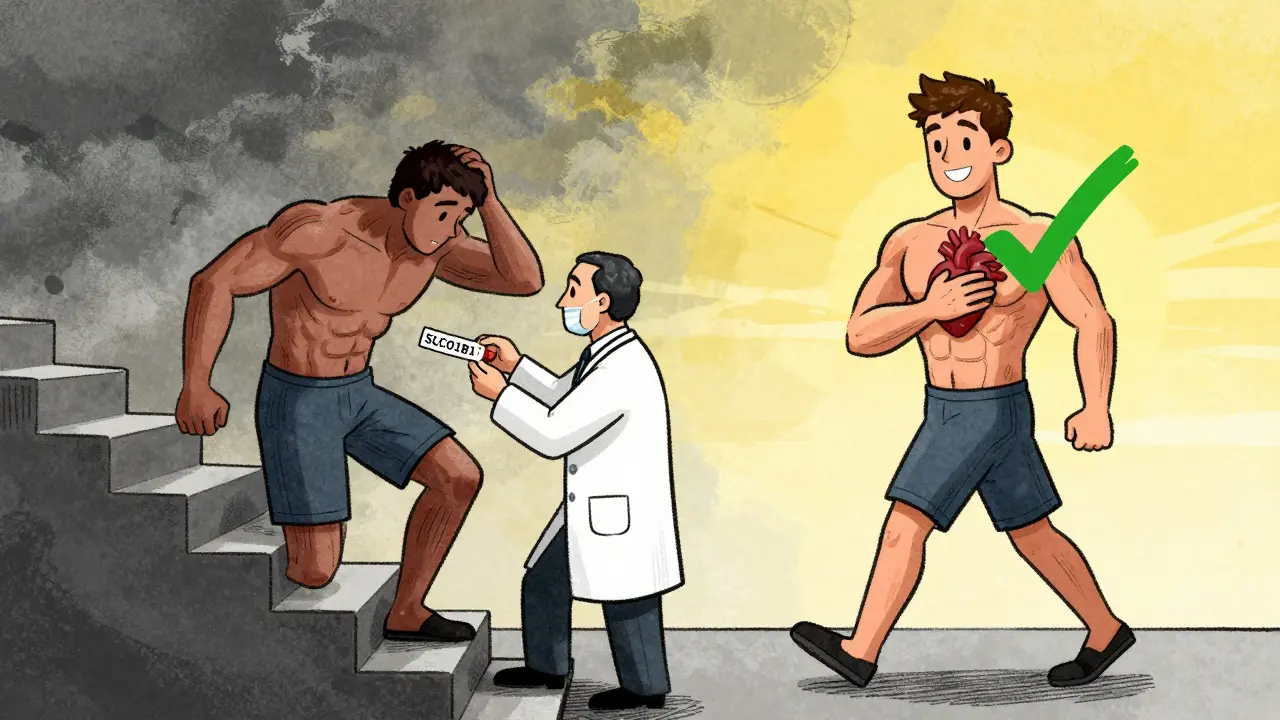
How to Stay Safe Long-Term
If you’re on a statin, here’s your simple safety checklist:- Know which statin you’re on. Is it simvastatin? That’s the riskiest.
- Never start a new antibiotic without checking if it interacts. Clarithromycin? Pause your statin.
- Get your CK checked if you have new muscle pain - especially after starting a new drug.
- Ask if you can switch to pravastatin or rosuvastatin. They’re safer with most meds.
- Don’t take gemfibrozil with any statin. Fenofibrate is fine.
- Keep a list of all your meds. Bring it to every appointment.








Fabio Raphael
24 Dec 2025 at 19:09I’ve been on simvastatin for 6 years and never thought twice until my knee pain got bad enough to cancel my hiking trip. Turns out I was on clarithromycin for a sinus infection. My doctor didn’t even ask about my statin. I felt dumb for not speaking up. Now I keep a printed med list in my wallet. Small change, huge difference.
Also, my CK was 8x normal. They told me to stop the statin cold. I was terrified. But after 3 weeks, I switched to rosuvastatin 10mg and the pain vanished. No more fear of stairs. Just wish more docs knew this stuff.
Thanks for posting this. It’s like someone finally translated the medical jargon into something real.