Vancomycin Risk Assessment Tool
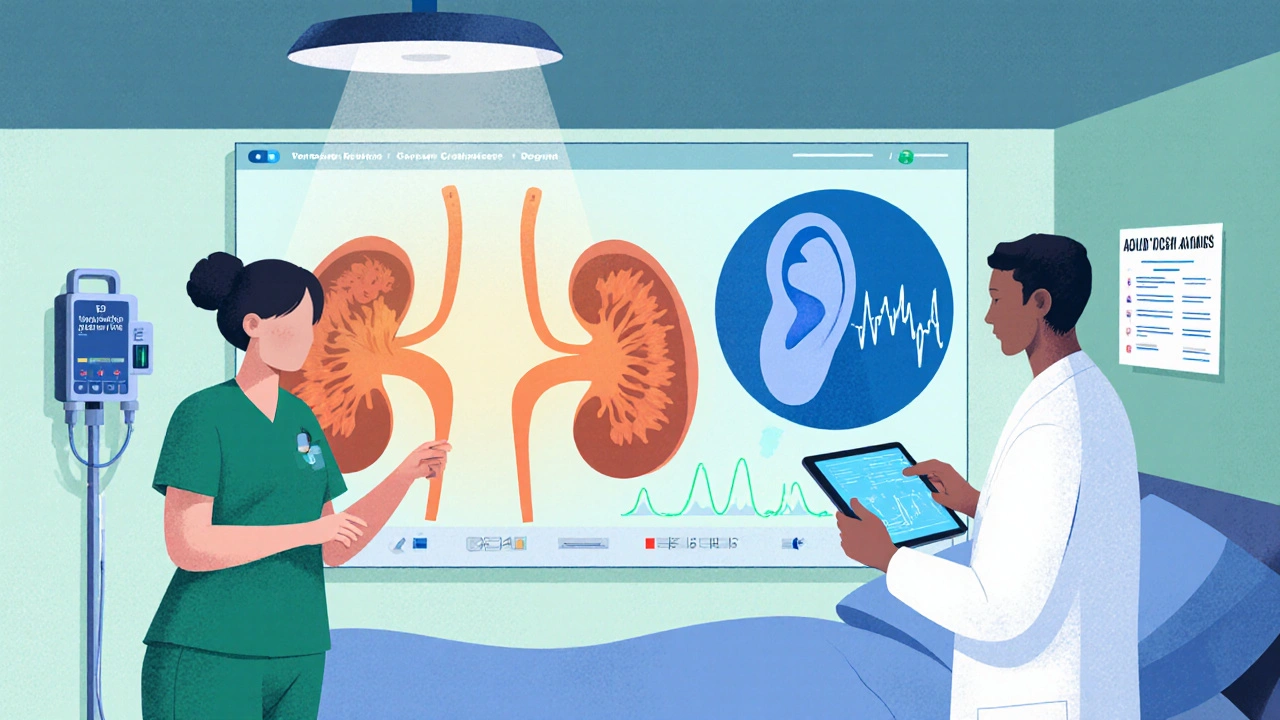
This tool calculates your patient's risk for vancomycin-induced nephrotoxicity and ototoxicity based on clinical factors. The risk score helps guide monitoring intensity and dose decisions.
Nephrotoxicity Risk Factors
Ototoxicity Risk Factors
Risk Assessment Results
Nephrotoxicity Risk Score
Ototoxicity Risk Score
Recommendations
When you prescribe Vancomycin is a glycopeptide antibiotic used for serious Gram‑positive infections, especially MRSA. While it saves lives, it also brings two nasty side effects - kidney injury and hearing loss. Figuring out which risk matters more for a given patient is the daily puzzle for infectious‑disease physicians, pharmacists, and hospitalists.
What’s the difference between nephrotoxicity and ototoxicity?
Both are drug‑induced injuries, but they hit different organs and follow distinct timelines.
- Nephrotoxicity - damage to the kidney’s proximal tubules, usually showing up as a rise in serum creatinine.
- Ototoxicity - injury to the inner ear’s hair cells, leading to high‑frequency hearing loss, tinnitus, or vertigo.
Nephrotoxicity is more common (5‑30% of patients depending on definitions), ototoxicity is rarer (about 1‑3%) but can be permanent.
How often does each toxicity occur today?
Historical data from the 1960s showed kidney injury rates over 50% because early drug lots contained impurities. Modern manufacturing and better dosing cut that dramatically, yet recent meta‑analyses still quote a 15‑25% AKI incidence for vancomycin alone and up to 30‑50% when paired with other nephrotoxins.
Hearing loss numbers are smaller but not negligible. A 2017 study found 12% of patients had high‑frequency loss, while a 2023 case report described rapid ototoxicity after just three therapeutic doses.
| Aspect | Nephrotoxicity | Ototoxicity |
|---|---|---|
| Typical incidence | 5‑30% (higher with combination therapy) | 1‑3% (higher with peak >40 µg/mL) |
| Time to onset | Days 3‑14 | During therapy or up to 72 h after stop |
| Reversibility | Usually reversible with prompt drug stop | Often permanent if peak >80 µg/mL |
| Key monitoring test | Serum creatinine, urine output | Audiogram, high‑frequency audiometry |
| Cost impact | ≈ 3 extra hospital days (≈ $5‑8k) | Long‑term hearing rehab $25‑50k/yr |
Major risk factors for kidney injury
Knowing the triggers lets you lower the odds before the lab values rise.
- Serum trough >15‑20 µg/mL - the risk curve steepens dramatically above 15 µg/mL (Rybak 2020).
- Daily dose ≥4 g - linked to a 2.9‑fold higher odds of AKI (Lodise 2008).
- Combination with other nephrotoxins, especially piperacillin‑tazobactam. A 2022 meta‑analysis showed a 1.31‑fold increase in AKI risk versus vancomycin + meropenem.
- Pre‑existing renal impairment or critical illness (higher baseline creatinine, ICU stay).
- Prolonged therapy >7 days - cumulative exposure adds to tubular stress.
Mechanistically, vancomycin generates reactive oxygen species that damage mitochondrial function in proximal tubule cells.
Major risk factors for hearing loss
Ototoxicity doesn’t care as much about other drugs; it watches peak concentrations and individual susceptibility.
- Peak serum >40 µg/mL - reversible loss tends to appear.
- Peak >80 µg/mL - irreversible injury reported.
- Genetic predisposition - MT‑RNR1 variants raise risk >3‑fold (Nature Communications 2022).
- Concurrent ototoxic meds (aminoglycosides, loop diuretics).
- Age >65 or pre‑existing hearing loss - baseline vulnerability.
Unlike kidney injury, there’s no reliable lab marker. Symptoms often show up as tinnitus or difficulty hearing high‑frequency sounds, which can be missed without formal audiometry.
How to monitor - kidney vs ear
Guidelines from the American Society of Health‑System Pharmacists (ASHP 2020) and the Infectious Diseases Society of America (IDSA 2021) give clear checkpoints.
- Nephrotoxicity monitoring
- Baseline serum creatinine and eGFR before first dose.
- Repeat creatinine every 48‑72 hours for the first two weeks.
- Switch to area‑under‑the‑curve (AUC) dosing when possible - studies show AUC‑guided regimens cut AKI from 14.7% to 8.2%.
- Flag any rise >0.3 mg/dL within 48 h as possible AKI (AKIN criteria).
- Ototoxicity monitoring
- Baseline audiogram before starting high‑dose (>4 g/day) or prolonged therapy (>7 days).
- Weekly high‑frequency audiometry for the same high‑risk groups.
- Document any new tinnitus, vertigo, or difficulty hearing high‑pitch sounds immediately.
- If peak levels exceed 40 µg/mL, consider dose reduction or alternative agent even if creatinine is stable.
Electronic health‑record alerts have already reduced vancomycin + piperacillin‑tazobactam use by 22% in hospitals that adopted them. Similar alerts for peak levels could help catch ototoxicity early, but they are still experimental.
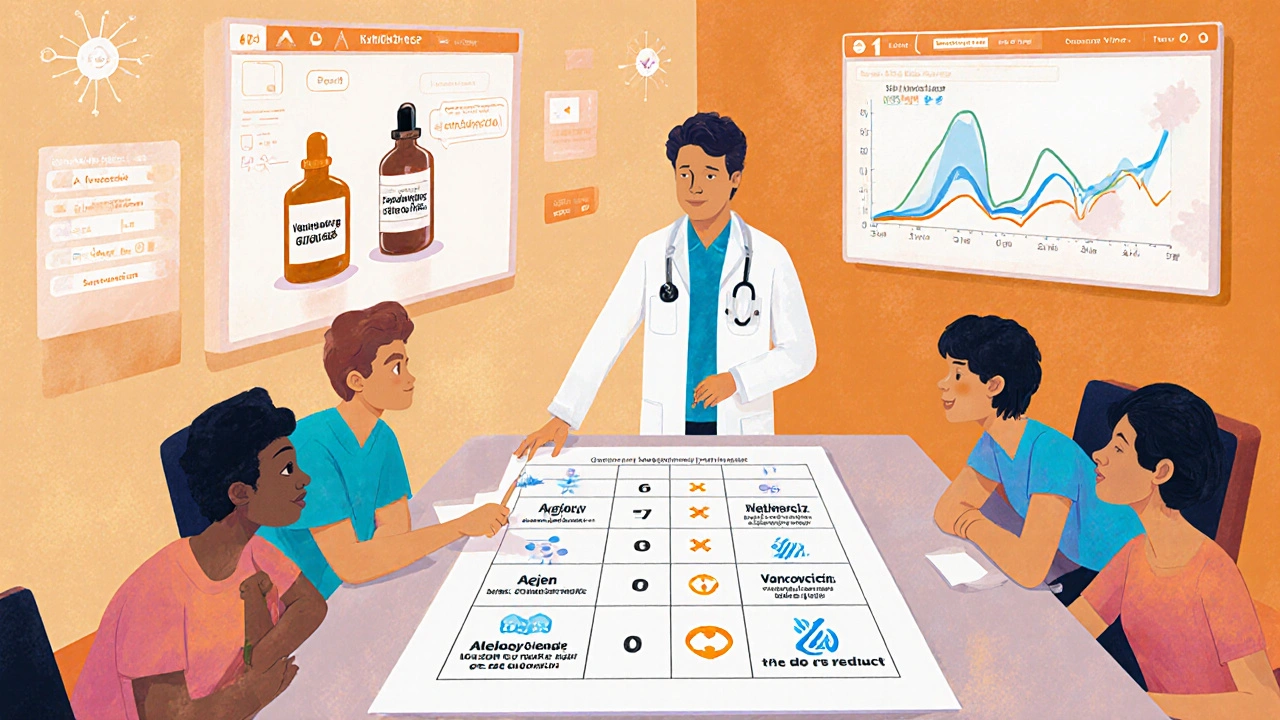
Balancing the two risks - decision framework
Think of toxicity as a scale. You weigh the patient’s infection severity, the need for high concentrations, and the presence of other drugs. The 2023 Society of Critical Care Medicine consensus sketched a three‑tier risk score (0‑8 points). Points are added for age >65, eGFR <60, combination therapy, dose >4 g, and known MT‑RNR1 variant.
| Risk factor | Points |
|---|---|
| Age >65 | 1 |
| eGFR <60 mL/min | 2 |
| Concurrent nephrotoxin (e.g., piperacillin‑tazobactam) | 2 |
| Daily dose ≥4 g | 1 |
| MT‑RNR1 variant | 2 |
Score 0‑2 = low risk - continue standard dosing, monitor creatinine twice weekly.
Score 3‑4 = medium risk - shift to AUC‑guided dosing, consider baseline audiogram.
Score ≥5 = high risk - look for alternatives (daptomycin, linezolid) unless vancomycin is absolutely required.
Practical tips for clinicians
- Target troughs of 10‑15 µg/mL for most infections; only push to 15‑20 µg/mL for hard‑to‑treat MRSA where AUC/MIC data support it.
- Prefer AUC monitoring over trough‑only - many institutions have switched after the 2021 VAN‑GUARD trial showed a 50% AKI reduction.
- If you must combine with piperacillin‑tazobactam, add a renal‑protective protocol: hydrate, limit vancomycin daily dose, and check creatinine daily.
- For patients >65 y, with baseline hearing loss, or on other ototoxins, order a baseline audiogram and repeat weekly.
- Document any subjective hearing changes right away - patients often describe “ringing” or “muffled sounds.” Early stop can prevent permanent loss.
When to switch away from vancomycin
Even the best monitoring can’t guarantee safety in every case. Consider an alternative if any of the following appear:
- Creatinine rises >0.5 mg/dL within 48 hours despite dose adjustment.
- Peak serum >80 µg/mL or sustained >40 µg/mL with emerging tinnitus.
- Patient meets high‑risk score (≥5) and an equally effective non‑glycopeptide is available.
- Allergic reaction or red‑man syndrome develops.
Alternatives such as daptomycin, ceftaroline, or linezolid each have their own safety profiles, so a quick side‑by‑side check is advisable.
Future directions - making vancomycin safer
Research is pushing toward personalized dosing. Pharmacogenomics (MT‑RNR1) may soon be a routine pre‑emptive test for patients slated for high‑dose therapy. Real‑time decision‑support platforms like DoseMeRx already integrate renal trends with AUC calculations, achieving 86% accuracy in predicting AKI.
On the ototoxicity front, point‑of‑care audiometry devices are being piloted in ICU settings, aiming to catch high‑frequency loss within hours instead of days. New vancomycin formulations with reduced impurity load are in late‑stage trials, hoping to lower both kidney and ear toxicity.
Until those tools become standard, clinicians must stay vigilant, balance dose intensity against the two toxicity scales, and keep communication open with pharmacists and audiologists.
What trough level of vancomycin is considered safe for the kidneys?
Current ASHP guidelines advise keeping troughs between 10‑15 µg/mL for most infections. Levels above 15‑20 µg/mL markedly increase AKI risk without adding efficacy.
How often should creatinine be checked during vancomycin therapy?
Baseline, then every 48‑72 hours for the first two weeks, or more frequently if the patient has existing renal disease or is on other nephrotoxic drugs.
Is routine audiometry required for every patient on vancomycin?
No. Baseline and weekly audiograms are recommended only for high‑dose (>4 g/day), prolonged (>7 days), or high‑risk patients (age >65, prior hearing loss, concurrent ototoxins).
Does combining vancomycin with piperacillin‑tazobactam increase ototoxicity?
The main synergy is renal; data show a higher AKI rate. Direct ototoxicity synergy is not well documented, but the combination can raise serum levels, indirectly affecting the ear.
When should I switch to an alternative to vancomycin?
Consider a switch if AKI develops despite dose adjustment, if peak levels exceed 80 µg/mL with hearing symptoms, or if the patient scores high on a toxicity‑risk rubric (≥5 points) and an effective alternative exists.






Barna Buxbaum
26 Oct 2025 at 17:10I’ve found that targeting an AUC/MIC ratio rather than a trough level can really trim the AKI odds, especially when you’re dealing with a patient who’s already on piperacillin‑tazobactam. Keeping the AUC between 400‑600 mg·h/L usually does the trick without sacrificing efficacy. Also, remember to flag any rise in serum creatinine of >0.3 mg/dL within 48 h – that’s the AKIN signal we all watch. For the ears, a baseline audiogram for high‑dose or prolonged courses saves a lot of grief later. Lastly, involving the pharmacy team early on helps set up those AUC‑based dosing tools before the first dose hits.